Understanding the Benefits Administration Process
This section discusses:
The Benefits Administration process.
Open enrollment.
Event maintenance.
The Snapshot process.
You use the PeopleSoft Benefits Administration process to perform:
Open enrollment.
Event maintenance.
The Snapshot process.
Both open enrollment and event maintenance involve a similar cycle of procedures:
Determination of participant benefits eligibility.
Calculation of benefit costs and flexible credits.
Creation and delivery of participant enrollment forms.
Data entry of participant election choices.
Validation of employee elections.
Analysis of processing, enrollment, and election data.
Loading of elections to the database.
Creation and delivery of election confirmation forms.
You use open enrollment for periodic benefits reenrollment across your employee population.
Open enrollment begins by determining the benefit program under which each participant should be managed and the benefit options available to participants, including associated prices and flexible credits. It also identifies default enrollments for participants, such as new hires, who have no current elections, but who are eligible for a benefit program.
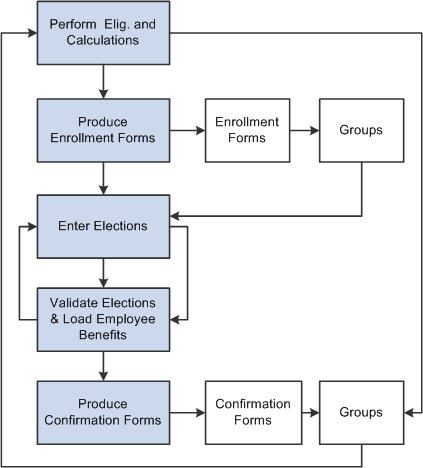
Elections are loaded as they are successfully validated. If problems or errors occur, individual participant elections can be rolled back, updated, and reloaded as necessary until the process is finalized. This diagram describes open enrollment processing:
Image: Open enrollment processing for periodic benefits reenrollment across your employee population
This image describes the open enrollment processing for periodic benefits reenrollment across your employee population.
You use event maintenance to process changes during the plan year and the enrollment of new hires. You might perform event maintenance every day, twice a week, or three times a month—whatever is necessary to properly react to changes in employee eligibility, process new hires, and update payroll benefit deductions.
Event maintenance identifies participant events that have occurred since the last run of the process that may change the benefits eligibility of the participant associated with the event. These events can include:
Family status events, such as divorce.
Job-related information changes, such as changes to pay frequency.
Passive events, such as the reaching of the age of retirement.
The hiring and termination of employees.
After event maintenance identifies employees who are associated with these events, it determines their current benefits eligibility according to the event and eligibility rules you've defined (assigning them new programs or plans as appropriate) and calculates benefit prices and flexible credits for their eligible options.
From this point on, event maintenance follows the same track as open enrollment.
Event Maintenance and COBRA Administration
PeopleSoft Benefits Administration initiates qualifying COBRA (Consolidate Omnibus Budget Reconciliation Act) events during the Event Maintenance process when a recognized COBRA event is finalized. The only exception to this rule is the Overage Dependent event, which is initiated by the COBRA process for both the Manage Base Benefits business process and Benefits Administration clients.
When Benefits Administration initiates the COBRA event, it populates the COBRA Activity table with the employee ID, employment record number, COBRA event date, COBRA action code (as defined on the Action Reason table) and event ID related to the initiated event. From that point, the activity (event trigger) is further processed only by the COBRA Administration system, not by Benefits Administration.
Before you begin using PeopleSoft Benefits Administration, you should establish an initial snapshot of your employees' current benefits eligibility. You can use the Open Enrollment process for this purpose. But if your first process is Event Maintenance, you need to use the Snapshot process first to establish a basis for managing subsequent changes in eligibility.
Essentially, the snapshot:
Compares employees' current data to the defined eligibility rules.
Records the options for which participants are currently eligible.
Flags instances in which employees are ineligible for their current enrollments.
The process finishes in a single run of the Benefits Administration background process and does not calculate costs or change current benefit enrollment information. It assigns all employees a snapshot event that the system closes with a finalized status at the end of processing.
Other Uses of the Snapshot
Because the Snapshot process looks at your entire workforce, you can also use the Snapshot process to:
Test your eligibility rule setup to find employees considered ineligible for their current benefits.
Establish default coverages and credits for which employee input isn't necessary (because the Snapshot process can optionally update employee election data).
Perform a final check of cost calculations by randomly selecting participants and coverages to track.
Validate the loading of legacy benefits data by comparing current enrollments established by your old system against eligible options determined by Benefits Administration.
Provided extensions to the Snapshot process can help accomplish these tasks. You can specify the features that you want on the Snapshot Definition page. If you have limited time for your conversion activity, then you can use these features on a test database and go to the basic version when you make your actual conversion to Benefits Administration.