Managing Nonemployee COBRA Participants
When a COBRA-qualified dependent selects individual coverage after an initial event or undergoes an event that involves a loss of dependent status, that dependent becomes a nonemployee COBRA participant. Nonemployee COBRA participants can declare their own dependents and change benefit programs and plans.
This section describes how to manage non-employee COBRA participants.
Note: When you add a nonemployee through COBRA, the nonemployee record may not show in other PeopleSoft HR processes until the Refresh Personal Data process is run.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
Name and Contact |
PERSONAL_DATA1 |
Update COBRA-qualified dependent name and biographical information. |
|
CBR_PERSONAL_DATA3 |
Maintain department security information for nonemployee COBRA participants. |
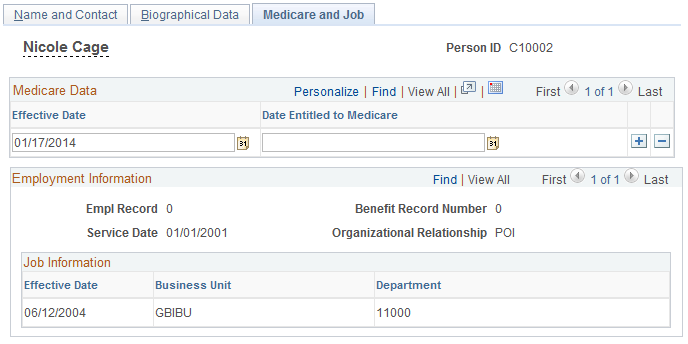
Use the Medicare and Job page (CBR_PERSONAL_DATA3) to maintain department security information for nonemployee COBRA participants.
Navigation:
This example illustrates the fields and controls on the Medicare and Job page. You can find definitions for the fields and controls later on this page.
Field or Control |
Description |
|---|---|
Employment Information |
During the COBRA processing, automatically populated with the original data of the employee that experienced the COBRA event. |
Job Information |
Review and update a historical record of the nonemployee participant's business unit and department affiliations. |
When a spouse or ex-spouse COBRA participant enrolls in individual nonemployee COBRA coverage, the child dependents of the employee are inherited as dependents for the nonemployee.
All nonemployee participants are assigned a unique system-generated employee ID for which the numbering convention is established in the Installation Table. All dependents of the nonemployee participant also have this new COBRA employee ID, along with their original dependent/beneficiary ID.
When a secondary event occurs, however, all of an employee's dependents become independently covered. For example, a former employee elects COBRA coverage for himself, his spouse, and his child. He later dies, which qualifies as a secondary event for the dependents. The spouse and child become nonemployee participants, and are assigned IDs as shown in the following table.
|
Person |
Employee ID |
Dependent/Beneficiary ID |
|---|---|---|
|
Employee (Deceased) |
Z001 |
00 |
|
Spouse (Nonemployee) |
C00015 |
01 |
|
Child (Nonemployee) |
C00016 |
02 |
If no further action is taken, the system creates COBRA health benefit records with employee-only coverage for the spouse and dependents, with their COBRA coverage extended to a total of 36 months from the initial event.
However, the spouse can also enroll the children as dependents under her coverage. To change from independent coverage for nonemployees to dependent coverage, follow these steps.
To convert nonemployee independent coverage to nonemployee dependent coverage:
Access the COBRA health benefit record for the nonemployee who is remaining independently covered.
Change the coverage code to an appropriate coverage code for dependent coverage for the plan types affected and add the dependent IDs to cover.
Access the Participation Termination page and create Voluntary Termination records for the dependents who are now covered under the spouse. The termination date for each termination record should be the same date that dependent coverage begins.