Determining Qualified COBRA Events
This section provides an overview of COBRA events and discusses how to determine qualified COBRA events.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
COBRA_ACTIVITY |
Add, delete, and review COBRA events. |
A qualified COBRA event:
Is defined in the COBRA Event Rules Table.
Results in a recognized loss of coverage in a health or FSA plan.
In the Manage Base Benefits business process, qualifying events are triggered through PeopleCode. In PeopleSoft Benefits Administration, qualifying events are triggered after Event Maintenance has been finalized. The exception (for both the Manage Base Benefits business process and Benefits Administration) is overage dependent processing. Overage dependent events are identified during the COBRA batch process and are automatically adjusted.
Information about triggered events is transferred to the COBRA Activity table for further analysis during the COBRA process.
Two types of COBRA events exist: initial and secondary. An initial event is the first qualifying event for an employee.
Understanding Initial COBRA Events
The following table shows the initial qualifying COBRA events that PeopleSoft software delivers, the user actions that trigger them, and the potential COBRA beneficiaries of each event.
|
Qualifying COBRA Event |
User Action Trigger |
Potential COBRA Beneficiaries |
|---|---|---|
|
Loss of eligibility due to termination |
Employee status changes to Terminated or Suspended. |
Employee and dependents |
|
Loss of eligibility due to reduction in hours |
Employee status remains Active; standard hours decrease. |
Employee and dependents |
|
Loss of eligibility due to retirement |
Employee status changes to Retired. |
Employee and dependents |
|
Loss of eligibility due to military leave |
Leave of Absence/Military Leave action/action reason combination is entered for the employee. |
Employee and dependents |
|
Death of employee |
Employee status changes to Deceased or a Family Status Change/Death action/action reason combination is entered for an employee. |
All dependents |
|
Divorce |
Marital status changes to Divorced; spouse becomes ex-spouse. |
Spouse |
|
Marriage of dependent |
Dependent marital status changes to Married. |
Individual dependent |
|
Dependent reaches coverage age limit (overage dependent) |
No user action; current age of dependent exceeds maximum dependent age or maximum student dependent age. (The system checks whether the dependent is a student.) |
Individual dependent |
|
Employee becomes entitled to Medicare |
Medicare entitlement date is entered. |
All dependents |
Note: According to federal government guidelines, employees who undergo voluntary or involuntary termination for gross misconduct and their spouses are not eligible for COBRA coverage. COBRA Administration does not differentiate between terminations for gross misconduct and other termination types, but you can set up action reason codes and add PeopleCode to perform this function.
Understanding Secondary COBRA Events
Secondary events extend coverage eligibility and are limited to dependents who are currently enrolled in COBRA coverage. A secondary event must meet the following requirements:
The dependent must currently be enrolled in COBRA coverage as a result of an initial COBRA event.
The initial COBRA event must be associated with a change to an employee's job status (such as a reduction in hours, termination, or retirement), and the secondary event must involve loss of coverage for the employee's dependent (such as divorce, marriage of dependent, overage dependent, death of employee, or a Medicare entitlement).
The triggers for secondary events are identical to the triggers for initial events, with one exception: If the initial event is a termination and the secondary event is a death, you must use the delivered action/action reason combination of FSC/DEA (family status change/death) to successfully process the event.
Use the Review COBRA Triggers page (COBRA_ACTIVITY) to add, delete, and review COBRA events.
Navigation
Image: Review COBRA Triggers page: Activity tab
This example illustrates the fields and controls on the Review COBRA Triggers page: Activity tab. You can find definitions for the fields and controls later on this page.
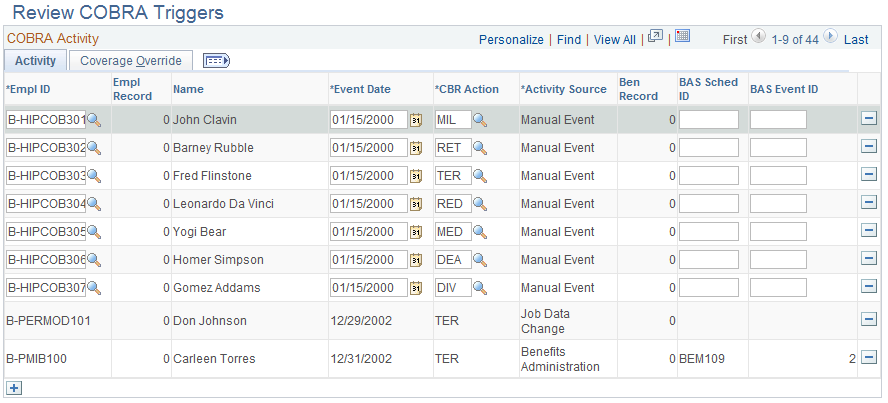
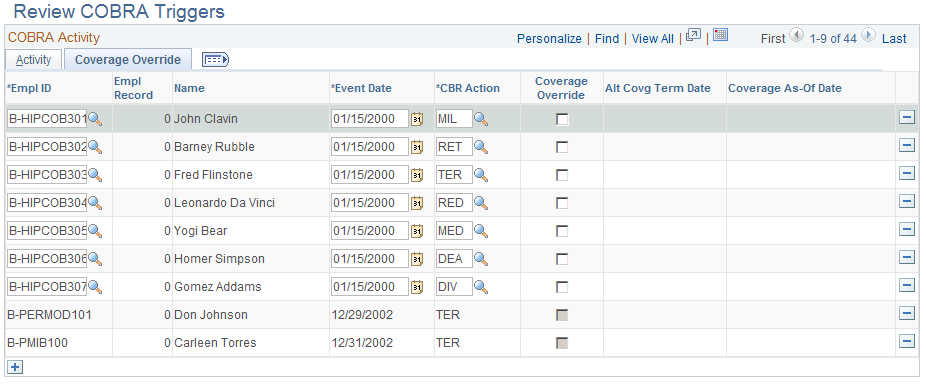
Image: Review COBRA Triggers page: Coverage Override tab
This example illustrates the fields and controls on the Review COBRA Triggers page: Coverage Override tab. You can find definitions for the fields and controls later on this page.
Activity Tab
|
Field or Control |
Definition |
|---|---|
| CBR Action (COBRA action) |
Describes the type of event that took place. |
| Activity Source |
Indicates who or what initiated the event. |
| Ben Record (benefit record number) |
Indicates the benefit record affected by the event. |
Coverage Override Tab
|
Field or Control |
Definition |
|---|---|
| Coverage Override |
Select when to use an alternate coverage termination date to determine qualified COBRA coverage. |
| Alt Covrg Term Date (alternate coverage termination date) |
The date when coverage was previously terminated. Required when the coverage override flag is selected. |
| Coverage As-Of Date |
The date that coverage should begin if the event is fully qualified. The system sets the COBRA event date if this field is left blank. |
The system assumes that the date of the event and the date that an employee's benefits terminate are the same, which is not always true.
For example, suppose that an employee drops spousal coverage during Open Enrollment and then later gets divorced. The benefit plan must make COBRA coverage available upon receiving notice of the divorce.
Another example is when an employee decides not to return to work from FMLA. COBRA coverage becomes available on the day human resources is notified that the employee is not returning, not on the last day of the FMLA, unless notification is made on the last day of FMLA. The maximum coverage period usually begins on that day also.
For the COBRA process to recognize these events as enabling dependents to become eligible for COBRA benefits, you must enter the event directly into the COBRA Activity Table.
You cannot enter an event unless you have selected Manual Events Allowed in the COBRA Event Rules Table for the COBRA event classification. You may want to add a new COBRA event classification to identify these specific situations. COBRA events triggered through the Manage Base Benefits business process or Benefits Administration can be deleted on the COBRA Activity Table, but not modified. COBRA events that you enter through the Review COBRA Triggers page can be changed.