Running the COBRA Process
This section provides an overview of the COBRA process and describes how to run it.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
COBRA_RUNCTL |
Run the COBRA process to determine eligibility. |
|
|
COBRA_MESSAGES |
View error messages for the COBRA process. |
The COBRA process determines employee and dependent eligibility for COBRA benefit coverage.
For an employee or dependent to become a qualified COBRA beneficiary, the following two requirements must be met:
The person must have experienced a qualifying event.
The person must have had health coverage on the day of the qualifying event and have lost coverage.
If these requirements are met, the COBRA process assigns the beneficiary a benefit program and allows that person to elect COBRA health coverage.
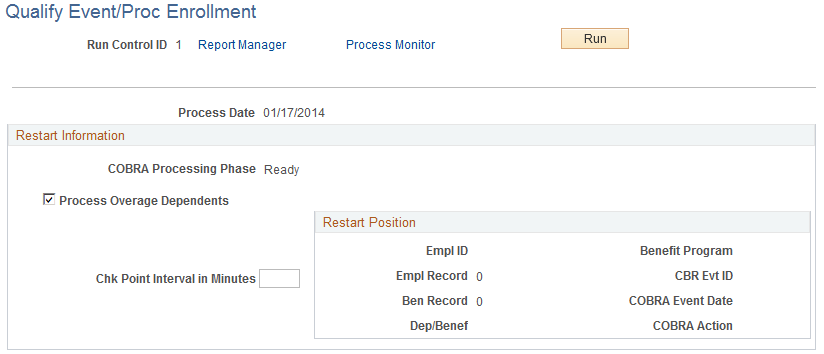
Use the Qualify Event/Proc Enrollment page (COBRA_RUNCTL) to run the COBRA process to determine eligibility.
Navigation
Image: Qualify Event/Proc Enrollment page
This example illustrates the fields and controls on the Qualify Event/Proc Enrollment page. You can find definitions for the fields and controls later on this page.
|
Field or Control |
Definition |
|---|---|
| COBRA Processing Phase |
Displays the phase where processing begins. Possible phases are: Ready: Ready for processing. Overage: Processing overage dependents. Activity: Processing COBRA activity. Qualify: Processing qualifying events. Participant: Processing COBRA participants. Complete: Processing completed. |
| Process Overage Dependents |
Deselect to skip overage-dependent processing during the batch run. |
| Chk Point Interval in Minutes (check point interval in minutes) |
Enter the number of minutes before the process commits information that's been processed so far and updates the information displayed in the Restart Position group box. If an error occurs, the system restarts the process from the last checkpoint. |
| Restart Position |
Displays the position from which to restart the COBRA process if a system failure occurs. |
Note: On the Process Scheduler page, select COBRA Admin & Non Employee to run the COBRA process. This runs both the COBRA Administration and COBRA Non Employee processes. The COBRA Administration process takes the relevant data and puts it into a temporary table. The COBRA Non Employee process writes the data to the correct PERSON table.
When a COBRA event has been triggered (online or through Benefits Administration), the COBRA process determines whether any employees or dependents have lost health coverage due to the event. The system considers these people to be qualified COBRA beneficiaries.
Each person analyzed by the COBRA process receives three status values:
Event qualification status
Initial event status
Secondary event status
The event qualification status identifies participants who qualify for COBRA. Statuses are:
Not COBRA Qualified
COBRA Qualify Error
COBRA Qualified
Qualify Pending
Unprocessed
The initial event status tracks the process of the event in the COBRA cycle; it also marks whether participants have their options prepared and are notified of coverage. Values include:
Qualify Pending
Qualified
Not Qualified
Options Prepared
Notified
Election Entered
Election Error
Election Enrolled
Enrollment Complete
The secondary event status is always Not Qualified unless the COBRA participant has been affected by a secondary event, such as divorce or Medicare entitlement. Other values include:
Qualify Pending
Qualified
Notified
Coverage Extended
When a participant is enrolled in COBRA coverage through an initial event and a qualified secondary event occurs for all of that participant's plans, the system sets the participant's initial event status to Not Qualified.
In the case of a combination event, which acts as an initial event for certain plans and as a secondary event for other plans, plans for which the combination event acts as a secondary event are set to Not Qualified. Initial event status values for plans for which the combination event acts as an initial event are set to appropriate levels for the current stage of processing.
Status values for initial and secondary events are updated as participants move through the COBRA process.
Benefit program assignment differs for COBRA events initiated by the Manage Base Benefits business process and Benefits Administration.
If a COBRA event is initiated by the Manage Base Benefits business process, the system assigns each qualified beneficiary to the benefit program that the employee was enrolled in on the day prior to the COBRA event date.
If the event is processed through Benefits Administration, then the system determines benefit program eligibility for each qualified COBRA beneficiary, using the eligibility parameters from the latest run of Benefits Administration and the qualified beneficiary's ZIP code. If no benefit programs satisfy this eligibility criteria, then the participant is assigned to the benefit program enrolled in on the day prior to the COBRA event date.
Note: This process occurs only for qualified participants who have a COBRA process status of Open For Processing (as opposed to Closed or Void).
Beneficiaries are eligible for all COBRA-qualified group health plan types that they were enrolled in prior to the COBRA event. This includes all Health (1x) plan types and the Health FSA (60) plan type.
For a plan type within a specific benefit program to be designated as COBRA-qualified, you must select the COBRA Plan check box in the Plan Type and Option page of the Benefit Program Table (BEN_PROG_DEFN) component.
Eligible options are determined for each qualified plan type.
For employees, spouses, and ex-spouses, eligible options must satisfy the following criteria:
The benefit plan associated with the options matches the benefit plan of the lost coverage of the employee, spouse, or ex-spouse.
The coverage code has the COBRA Coverage Set field selected and is less than or equal to the coverage code of the lost coverage of the employee, spouse, or ex-spouse.
For spouses and ex-spouses, the coverage code selected cannot require a spouse or ex-spouse (Spouse Only Coverage codes).
For all dependents besides spouses and ex-spouses, eligible options must satisfy the following criteria:
The benefit plan associated with the options matches the benefit plan of the dependent's lost coverage.
The dependent's coverage code is Employee Only (Dependent Only Coverage).
Note: The Employee Only code is used when the dependent is covered on his or her own and as a dependent of the COBRA participant. The code is used to indicate the coverage of a single person.
Benefits Administration uses a different method to determine option eligibility.
This section describes how to calculate COBRA costs.
To calculate COBRA cost:
Access the Benefit Program page.
Enter the COBRA percentage amount.
The COBRA process calculates a charge for each option using the sum of the total coverage costs (employee plus employer) multiplied by the surcharge defined here.
Enter the COBRA disabled surcharge percentage.
If the COBRA participant is disabled, the COBRA cost for months 19–29 is multiplied by this surcharge.
When you select Waive COBRA Surcharge on the COBRA Event Rules Table page for a specific COBRA event classification, the system does not add the COBRA surcharge or disabled surcharge.
COBRA charges are sent to the COBRA beneficiary through Benefits Billing processes, as long as Benefits Billing is selected in the Products page of the Installation table.
Although COBRA governmental regulations describe how secondary COBRA qualifying events should be processed, PeopleSoft event rules allow for a different implementation of secondary event processing.
Three fields defined on the Event Rules page are used to process secondary events.
|
Field or Control |
Definition |
|---|---|
| Secondary Event Role |
Identifies whether the event can be considered a secondary event. |
| Second Event Additional Months |
Defines by how many months the secondary event extends a COBRA participant's coverage. |
| Secondary Event Add Mode |
Defines whether the additional months extend the coverage 36 months from the coverage begin date of the initial event or add 36 months to the COBRA event date of the secondary event. |
Use the Review Processing Messages page (COBRA_MESSAGES) to view error messages for the COBRA process.
Navigation
|
Field or Control |
Definition |
|---|---|
| Benefit Rcd# (benefit record number) |
The employee benefit record number that was affected by the COBRA event. |
| CBR Evt ID (COBRA event identification) |
The identification number assigned to the event by the COBRA process. |
| Dep/Benef (dependents/beneficiaries) |
Any relevant dependents or beneficiaries. |