Creating Notification Letters
This section describes how to create notification letters.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
RUNCTL_CBR001 |
Print notification letters for initial COBRA events. |
|
|
RUNCTL_CBR002 |
Print notification letters for secondary COBRA events. |
|
|
CBR_PRT |
Select parameters for reprinting notification letters. |
The qualifying event determines recipients.
For termination, reduction in hours, and retirement events, the employee and each covered dependent are notified.
When Medicare entitlement or death of employee events occur, each dependent is notified.
When divorce or loss of dependent status events occur, the spouse or dependent is notified.
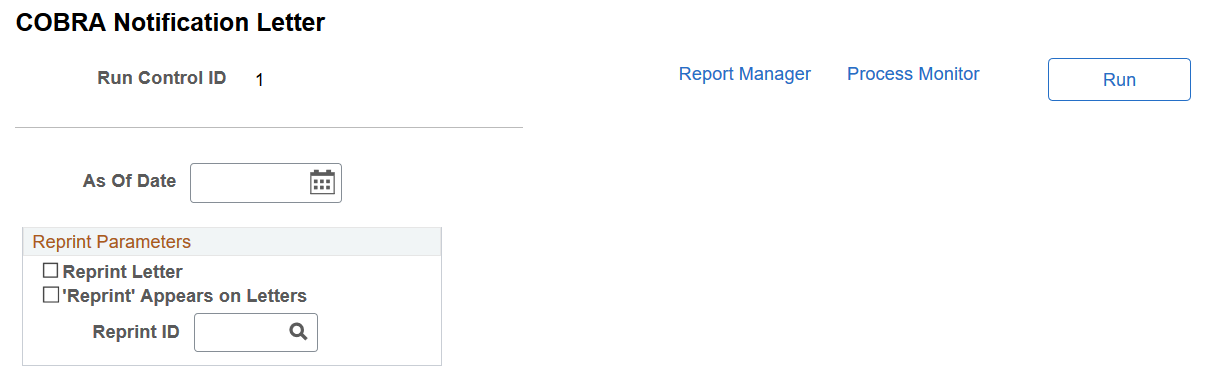
Use the COBRA Notification Letter page (RUNCTL_CBR001) to print notification letters for initial COBRA events.
Navigation:
This example illustrates the fields and controls on the COBRA Notification Letter page. You can find definitions for the fields and controls later on this page.
The Initial Notification Letter process generates letters for COBRA participants with an initial event status of Options Prepared and an event status of Open For Processing. Letters include:
The nature of the qualifying event and the date it occurred.
The last day of active coverage of the qualified participant's original benefit plans.
The plan types for which the qualified participant is eligible to receive COBRA coverage.
The COBRA coverage start and end dates for each plan, and the response date by which the qualified participant must notify you of his or her elections.
Along with each initial notification letter, the system prints a COBRA continuation coverage election form for employees to record their elections.
When an initial notification letter is generated for a qualified COBRA participant, the initial event status is changed to Notified. The election end date is calculated for each plan type as 60 days past the latter of the notification date (on the notification letter) or the loss of coverage.
Field or Control |
Description |
|---|---|
As Of Date |
Enter the date for the time period during which you want the letters. |
'Reprint' Appears on Letters |
Select this check box if you want the word Reprint to appear on the letter. |
Reprint ID |
Select the ID number associated with the letters that you want reprinted. |
Use the COBRA Secondary Letter page (RUNCTL_CBR002) to print notification letters for secondary COBRA events.
Navigation:
The process for printing notification letters for secondary events is identical to that for initial events.
The secondary notification letter includes information about how long COBRA coverage is to be extended.
Recipients have their secondary event status changed to Notified and their process status changed to Closed for Processing.
Use the Reprint COBRA Letter page (CBR_PRT) to select parameters for reprinting notification letters.
Navigation:
This example illustrates the fields and controls on the Reprint COBRA Letters page. You can find definitions for the fields and controls later on this page.
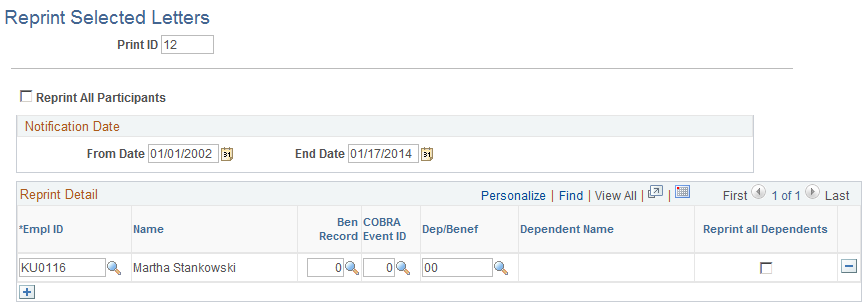
This page enables you to reprint all letters, or to select specific employees for whom letters are to be reprinted. You can specify a notification date range during which the reprint is to occur.