Value Based Care Dashboard
The Value Based Care Dashboard contains the following pages:
- Member Analysis
- PMPM Analysis
- Risk Score Analysis
- Rx Claim Analysis
- ACO Measures
- Patient Caregiver Experience
Parent topic: Oracle Healthcare Foundation Dashboards
Member Analysis
The Member Analysis page displays analytics based on the Member Month Eligibility and Medical Claim subject areas.
Figure 2-1 Member Analysis Page
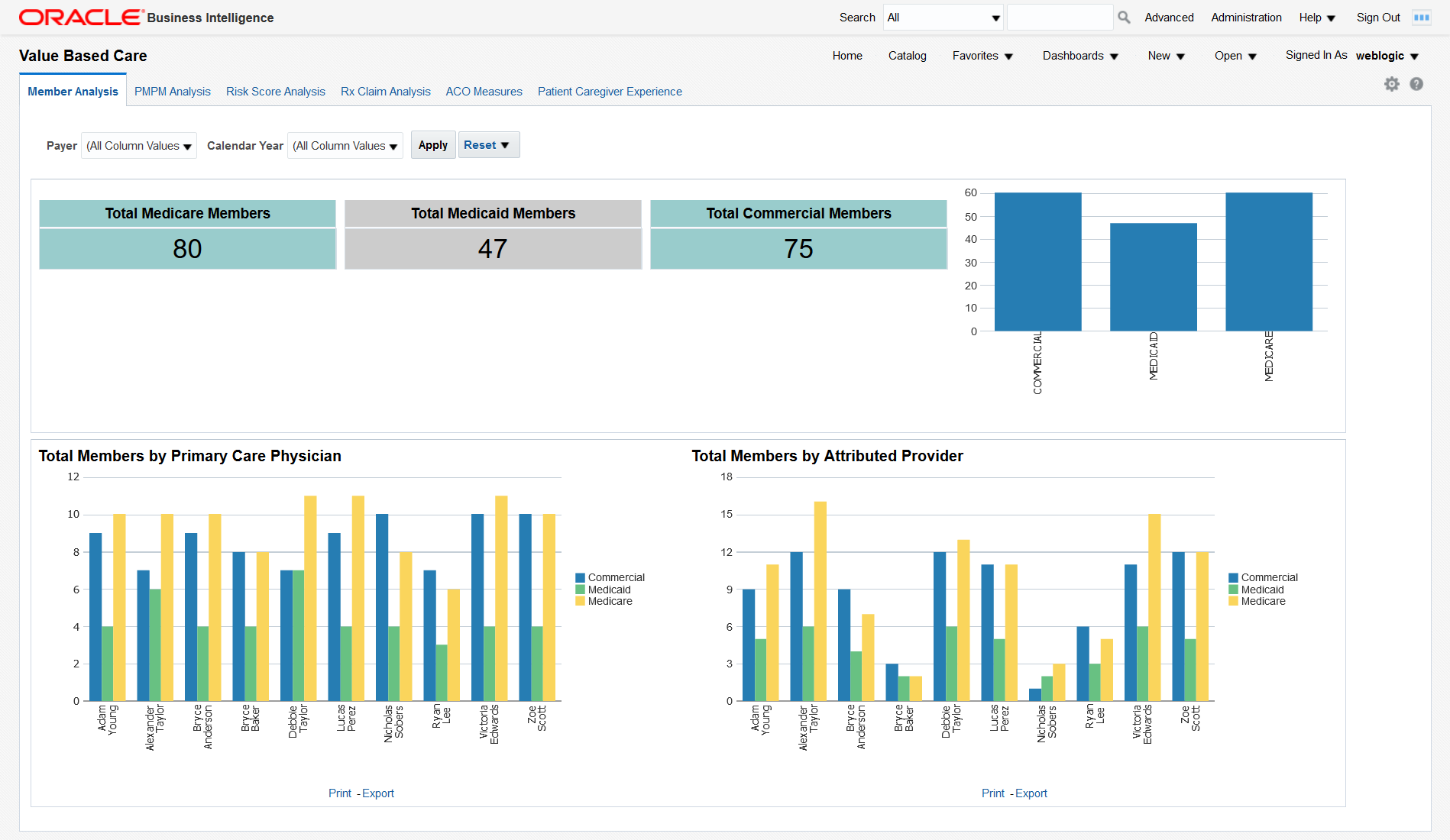
You can use the filters at the top of the page to focus on specific payers and calendar years. This page has the following reports:
- Total medicare, medicaid, and commercial members. This report shows the organization's exposure to different insurers based on the number of patients they cover. Click on the bars in the graph to display details about all the members covered by each insurer.
- Total Members by Primary Care Physician. This report shows each primary care physician's exposure to different insurers based on the number of patients they cover. Click on the bars in the graph to display details about all the members covered by each insurer for every primary care physician.
- Total Members by Attributed Provider. This report shows each attributed provider's exposure to different insurers based on the number of patients they cover. Click on the bars in the graph to display details about all the members covered by each insurer for every attributed provider.
Parent topic: Value Based Care Dashboard
PMPM Analysis
The PMPM Analysis page displays analytics based on the Member Month Eligibility, Medical Claim, and Rx Claim subject areas.
Figure 2-2 PMPM Analysis Page
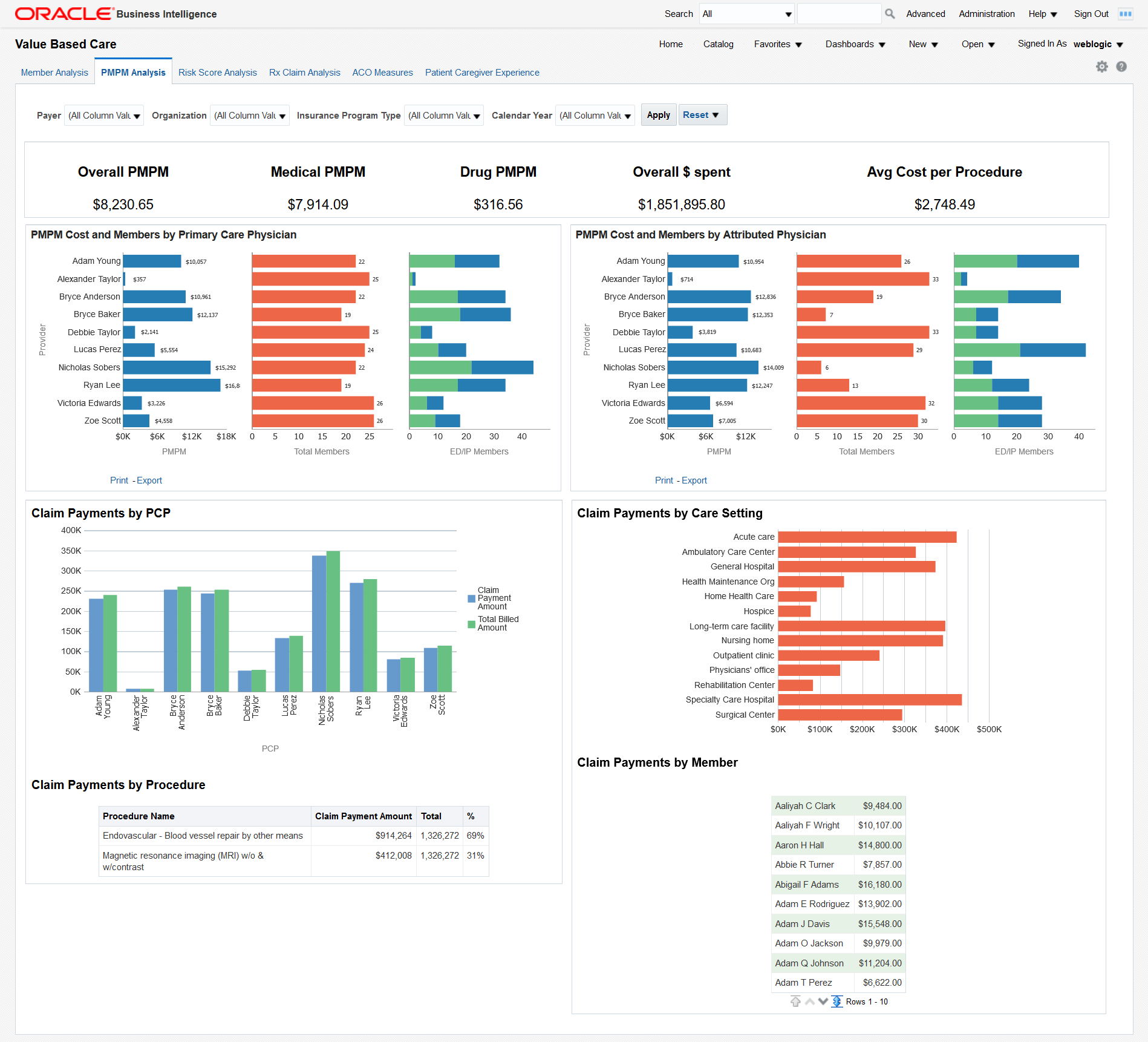
You can use the filters at the top of the page to focus on specific payers, organizations, insurance program types, and calendar years. This page has the following reports:
- PMPM overall, medical and drug cost in dollars, overall dollars spent, and average cost per procedure. This report allows you to see the average monthly costs per member and their distribution between medical and drug PMPM costs. It also allows you to evaluate your total costs and the cost of a typical procedure.
- PMPM Cost and Members by Attributed Physician. This report helps you understand the
PMPM costs that attributed physicians generate through the average monthly cost per
member and the total number of members assigned. The distribution between emergency
and inpatient members also helps you understand the associated costs.
Click any bar in the PMPM graph do display a detailed breakdown of all the amounts for each attributed physician.
- High Cost Members by Primary Care Physician. This report helps you understand the
costs that primary care physicians generate through the average monthly cost per
member and the total number of members assigned. The distribution between emergency
and inpatient members also helps to understand the associated costs.
Click any bar in the PMPM graph do display a detailed breakdown of all the amounts for each primary care physician.
- Claim Payments by PCP - Graphical representation of the claimed payment amounts and billed amounts by primary care physician. This report allows you to compare the overall payments claimed by primary care physicians and to check how they are covered by the billed amounts.
- Claim Payments by Procedure - A tabular report of the claim payments for each procedure compared to the total amount. The percentage helps you identify the procedures that generate the largest claims.
- Claim Payments by Care Setting - Graphical representation of the claim payment amounts for each case setting. This report helps you visualize the care settings that generate the largest claims.
- Claim Payments by Member - A tabular report that lists all members and their claim payments. This report allows you to drill down to the payments claimed for each member.
Parent topic: Value Based Care Dashboard
Risk Score Analysis
The Risk Score Analysis page displays analytics based on the Member Risk Score subject area.
Figure 2-3 Risk Score Analysis Page
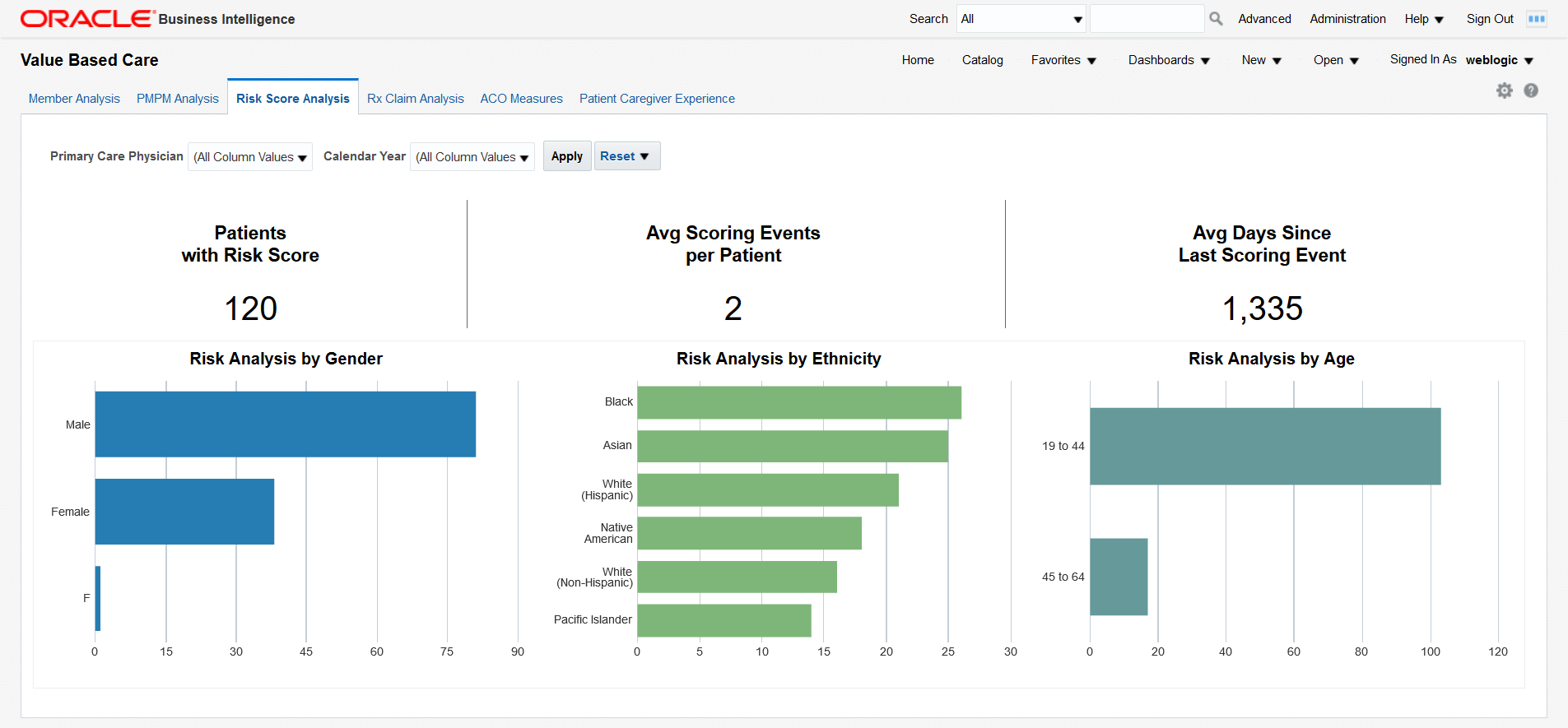
You can use the filters at the top of the page to focus on specific primary care physicians and calendar years. This page has the following reports:
- Total number of patients with risk score, average scoring events per patient and average days since last scoring event. This report helps you understand the scoring activity volume based on the number of patients it is performed on, the number of scoring events per patient, and their frequency.
- Risk analysis by gender, ethnicity, and age. Correlate this report with the total numbers of patients in each category to understand which genders, ethnic groups, and age bands are more exposed to risks.
Parent topic: Value Based Care Dashboard
Rx Claim Analysis
The Rx Claim Analysis page displays analytics based on the Prescription Claim subject area.
Figure 2-4 Rx Claim Analysis Page
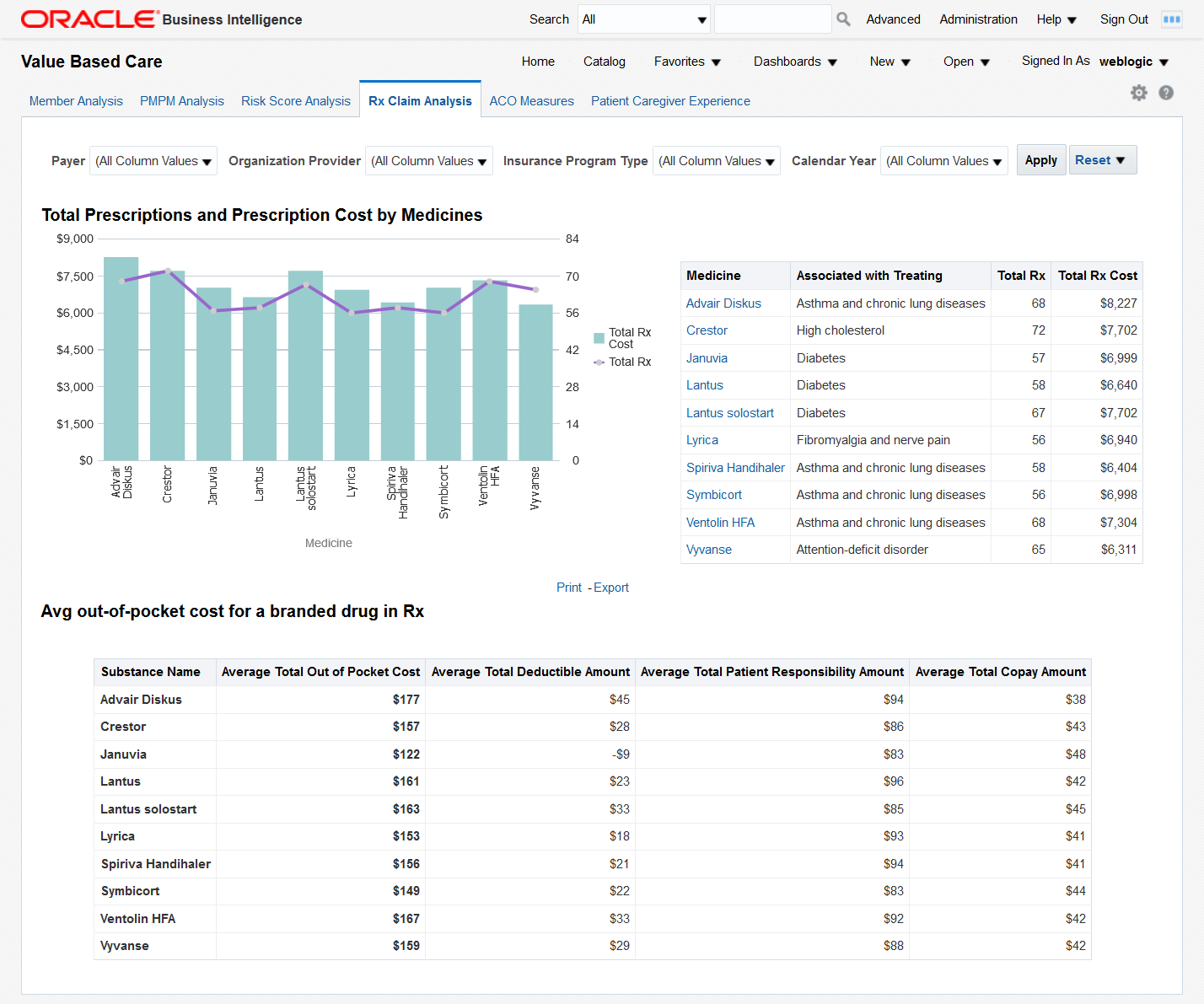
You can use the filters at the top of the page to focus on specific payers, organization providers, insurance program types, and calendar years. This page has the following reports:
- Total Prescriptions and Prescription Cost by Medicines - This report helps you
understand how often different medicines are prescribed and the costs that these
prescriptions generate.
Click on a bar or on a medicine name to display detailed prescription information for all the members who have been prescribed the medicine. There are 2 levels of drill down. Clicking further on the member number shows another detailed report for each member with Bill details.
- Avg out-of-pocket cost for a branded drug in Rx - Shows the average out of pocket cost that patients pay for a given set of medicines along with the breakdown of that cost by deductible, patient responsibility, and copay amounts.
Parent topic: Value Based Care Dashboard
ACO Measures
The ACO Measures page uses quality measurements based on the Accountable Care Organization (ACO) standards. You can customize this page to be used for any quality measure.
Figure 2-5 ACO Measures Page
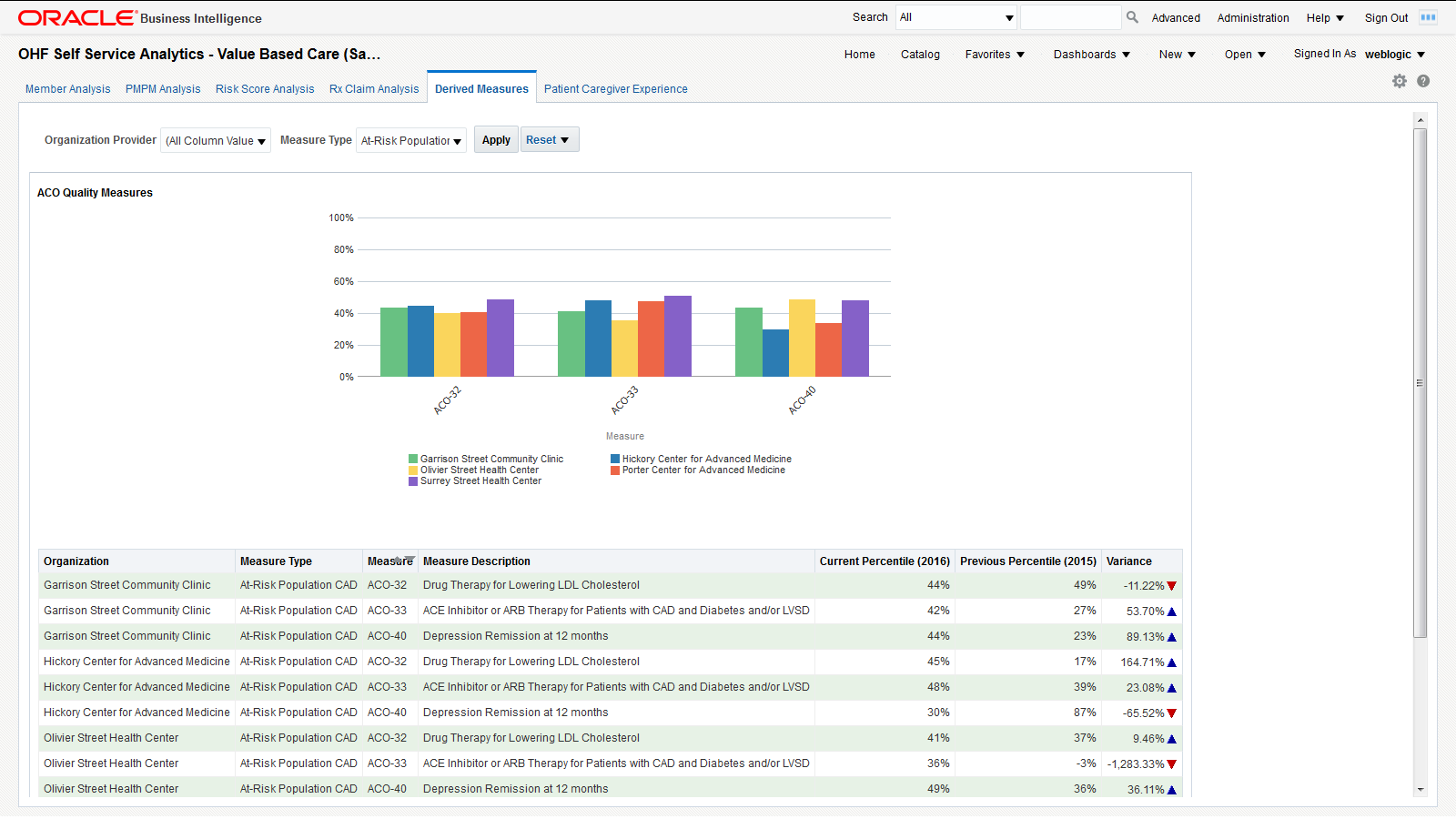
You can use the filters at the top of the page to focus on specific organization providers and measure types. This page has the following report:
- ACO Quality Measures - Graphical representation of the percentile rating for the selected organization providers for specific measure types. This report allows you to understand how organization providers compare to each other on different measures. The detailed tabular report below the chart also includes the percentile variance from the previous year to the current year, providing insight into the progress of an organization over different ACO quality measures.
Note:
The derived measure model supports drill-down to a patient, member, individual and organization service provider, encounter, internal organization, medical claim, and Rx claim from the quality measure results.Parent topic: Value Based Care Dashboard
Patient Caregiver Experience
The Patient Caregiver Experience page centralizes responses from patient surveys.
Figure 2-6 Patient Caregiver Experience Page

You can use the filters at the top of the page to focus on specific organization providers, departments, physicians, and calendar years. This page has the following report:
- Patient Satisfaction Survey - Shows the survey response results rolled up to the
categories, such as cleanliness of hospital environment, communication about
medicines, and communication with doctors and nurses. Click on a graph bar to
display the detailed answers for that survey category.
On the right side, the survey displays the performance score for each area. For example, "During the hospital stay, how often doctors explained in a way that the patient could understand?" has a score of 80%, which means 80% of patients agreed that the doctors explained clearly. Click on a percentage number to display the detailed answers for that survey question.
Parent topic: Value Based Care Dashboard