5.4.2 Claim Handling Tab
The Claim Handling tab includes information at the corporate level and focuses on the manner and quality by which the handling of a claim is measured.
The filters for this tab include:
- Time
- Company
- Geography
The various reports available for this tab are discussed in the following sections.
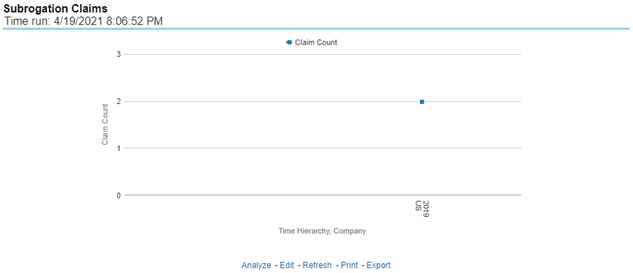
Average Days until Closed
Figure 5-195 Average Days until Closed
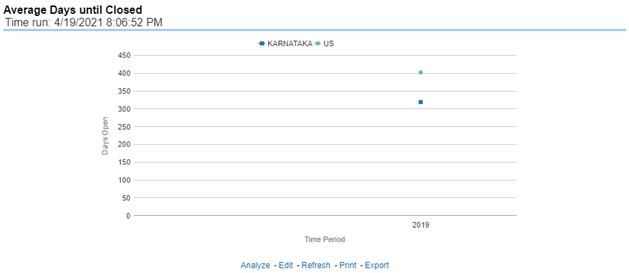
Closed Without Payment
This report is a line graph that illustrates the count of claims that were closed during the reporting period without any loss payments generated for the claim.
Figure 5-196 Closed Without Payment
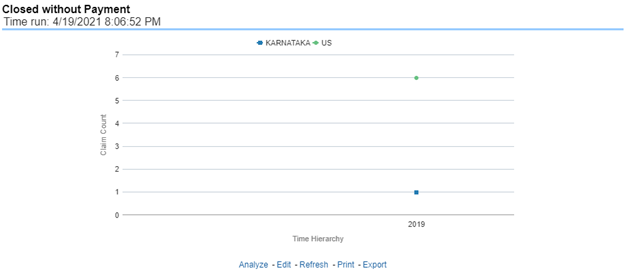
Claims Closed Due to Fraud
Figure 5-197 Claims Closed Due to Fraud
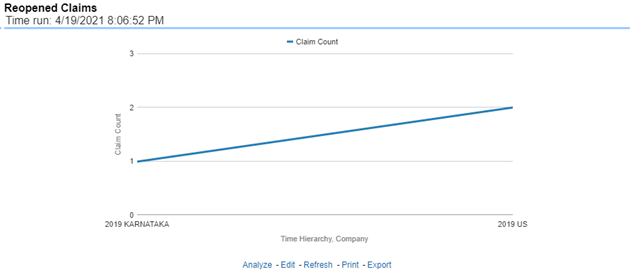
Reopened Claims
Figure 5-198 Reopened Claims
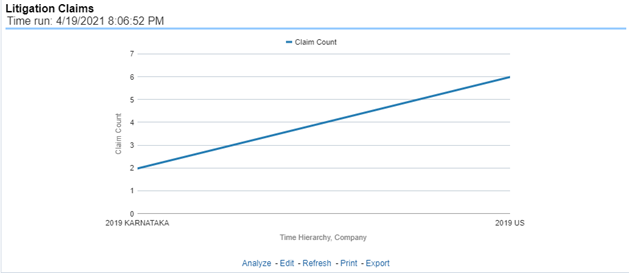
Litigation Claims
Figure 5-199 Litigation Claims
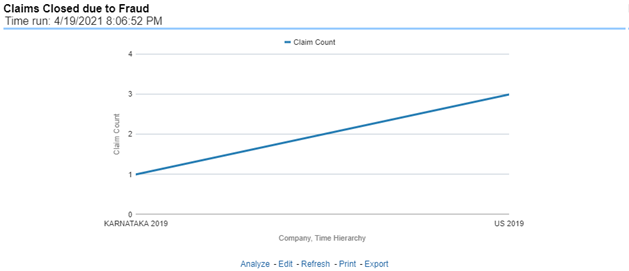
Subrogation Claims
Figure 5-200 Subrogation Claims