Enter Claim
This page is used to create new claims and to edit existing claims that have the status 'ENTRY'. The retrieval and display of data in this page is subject to restrictions described in the "User Access" chapter of the Security Guide.
Clicking the 'Enter Claim' button in the regional area will open a blank instance of this page in a dynamic tab. In addition, this page can be accessed through the Claims Search Result page on one of the search results. This will open an instance of this page in a dynamic tab for that particular claim.
This page has a similar layout to the other claim pages with the local area divided into four sections (Local Area);
-
Claim
-
Claim Details
-
Claim Line
-
Claim Line Details
Although the page has a similar layout, it contains some differences to support claim entry for example;
-
Hiding fields and details containing process data
-
Reordering fields and grouping mandatory fields
-
Representing all the claim fields in a single column
-
Automatically clearing the page after submitting a claim
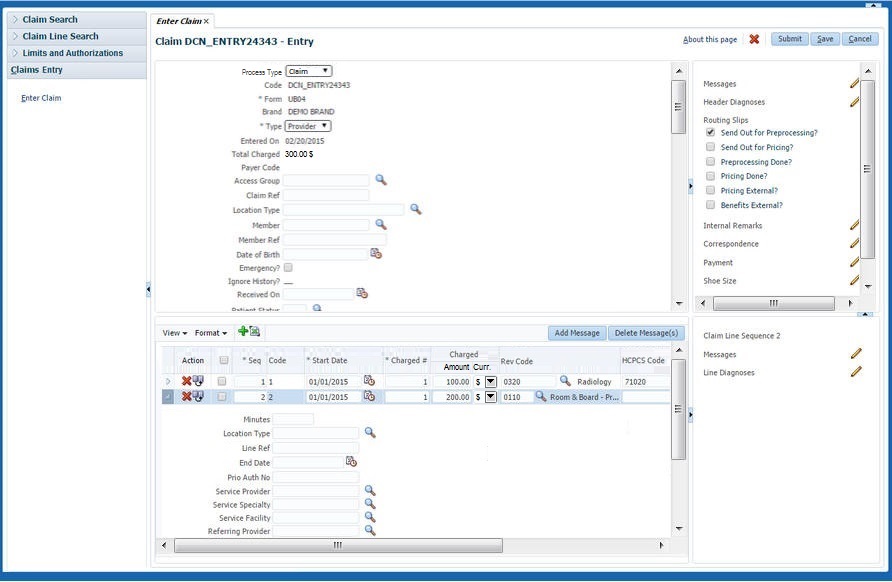
Claim Section
While entering a claim, field values are not checked for time validity as of the service date. These validations are executed during processing, not while entering the claim. This section displays the attributes of a single claim in a form based layout in a single column. The section holds the following fields:
| Display Label | Entity Field |
|---|---|
Process Type |
claim.processType |
Code |
claim.code |
Form |
claim.claimForm.code |
Brand |
claim.brand.code |
Type |
claim.type |
Entered on |
claim.entryDate |
Total Charged |
claim.totalClaimedAmount.amount and claim.totalClaimedAmount.currency.displayCode |
Payer Code |
claim.payerCode.code |
Access Group |
claim.dataAccessGroup.code |
Claim Ref |
claim.providerReference |
Claim Set |
claim.claimSet.code |
Emergency? |
claim.emergency |
Ignore History? |
claim.ignoreHistory |
Location Type |
claim.locationType.code |
+ description |
claim.locationType.description |
Entity Type |
|
Entity |
|
+ formatted name |
claim.servicedPerson.(formatted name) (Only for serviced entity type Person) |
+ gender |
claim.servicedPerson.gender (Only for serviced entity type Person) |
+ date of birth |
claim.servicedPerson.dateOfBirth (Only for serviced entity type Person) |
+ current address |
derived (Only for serviced entity type Person) |
+ description |
|
+ date |
|
Entity Ref |
claim.providerEntityReference |
Servicing Provider |
claim.serviceProvider.code |
+ (formatted) name |
claim.serviceProvider.(formatted)name |
Service Specialty |
claim.serviceSpecialty.code |
+ description |
claim.serviceSpecialty.description |
Service Facility |
claim.locationProvider.code |
+ (formatted) name |
claim.locationProvider.(formatted)name |
Referring Provider |
claim.referralProvider.code |
+ (formatted) name |
claim.referralProvider.(formatted)name |
Billing Provider |
claim.claimantProvider.code |
+ (formatted) name |
claim.claimantProvider.(formatted)name |
Billing Relation |
claim.claimantRelation.code |
+ (formatted) name |
claim.claimantRelation.(formatted)name |
Pay To Provider |
claim.paymentReceiverProvider.code |
+ (formatted) name |
claim.paymentReceiverProvider.(formatted)name |
Pay To Relation |
claim.paymentReceiverRelation.code |
+ (formatted) name |
claim.paymentReceiverRelation.(formatted)name |
Specification To Provider |
claim.paymentSpecificationReceiverProvider.code |
+ (formatted) name |
claim.paymentSpecificationReceiverProvider.(formatted)name |
Specification To Relation |
claim.paymentSpecificationReceiverRelation.code |
+ (formatted) name |
claim.paymentSpecificationReceiverRelation.(formatted)name |
Beneficiary Provider |
claim.paymentBeneficiaryProvider.code |
+ (formatted) name |
claim.paymentBeneficiaryProvider.(formatted)name |
Beneficiary Relation |
claim.paymentBeneficiaryRelation.code |
+ (formatted) name |
claim.paymentBeneficiaryRelation.(formatted)name |
Preceding Payer |
claim.precedingPayerCode |
Preceding Payer Paid on |
claim.paidDate |
Authorization |
claim.authorizationCode |
Received on |
claim.receiptDate |
Expires on |
claim.expirationDate |
The following claim fields are mandatory:
-
claim.processType (Process Type)
-
claim.form (Form)
-
claim.type (Type)
-
claim.ignoreHistory (Ignore History?). The checkbox value is defaulted by the value set in the property file for the instance (if not specified in the property file, it is defaulted to unchecked), but can be changed. In other words, if the property file settings for the ignore history indicator are specified correctly and no exceptions on claim level ever come in, then this value needs never to be changed manually.
When the claim.code (Code) is left empty, the system generates a unique claim code when saving the claim.
When entering a claim, the default value for the Emergency? check box is unchecked. When entering a claim the Indicator Manual is automatically checked, but this field is not shown. The Total Charged field is set by Claims and can never be edited directly.
This section contains dynamic fields that extend the claim table.
Claim Detail Section
For each claim detail, a list of records is shown. These lists show a selection of key fields per detail records, for example, if a claim has ten diagnoses then all ten are shown with only priority, type and code. In addition to detail records, this section also shows claim attributes that are expected to take up a lot of page real-estate (free form remarks, routing slips).
Nearly all summaries display an edit icon. Clicking this icon will open a dialog that shows all information available for that claim detail and allows the user to create details for that claim.
The subsections are listed in the same sequence as they appear (top to bottom) in the claim detail section:
| Displayed Header | Entity Field |
|---|---|
Financial Hold status and history |
FinancialHoldList[].FinancialHoldType.code FinancialHoldList[].status FinancialHoldList[].expirationDateTime Edit/View icon |
Messages |
claimMessageList[].message.severity claimMessageList[].message.code Edit/View icon |
Diagnoses |
claimDiagnosisList[].sequence claimDiagnosisList[].diagnosisType.description claimDiagnosisList[].diagnosis.code Edit/View icon |
Routing Slips |
claim.sendOutForPreprocessing claim.sendOutForPricing claim.preprocessingDone claim.externalPricing claim.externalBenefits |
Internal remarks |
claim.internalRemarks Edit/View icon |
External remarks |
claim.externalRemarks Edit/View icon |
Messages are sorted on code and diagnoses are sorted on sequence.
Financial Holds are sorted first on hold type, then on hold date. The most recent financial hold is listed first. The edit/view icon is controlled by access restriction Financial hold. This section is always visible even if there are no financial holds applied to the claim. When the edit or view button is clicked, a detailed page is opened in the context of the selected claim that shows all financial holds that were entered for the claim. When the user has edit privileges for financial holds, new financial holds can be entered in this page and existing financial holds can be released. When the view icon is pressed, the page is opened in display-only mode.
Routing slips are shown as checkboxes, one under each other, in the order as specified above. The indicators are editable. The indicators 'Send Out for Preprocessing?', 'Send Out for Pricing?' and 'Pricing External?' are checked by default, the others are unchecked by default.
Displaying External Claims Data
In addition to the listed 'fixed' detail summaries, the claim detail section also displays external claims data including the indicator 'Exempt from Purging?' which is shown as a checkbox. An external claims data entity serves as a container for dynamic fields and dynamic records that represent external information written to a claim in Claims.
External claims data is displayed as follows; each dynamic record usage and each dynamic field usage represent as a separate detail summary. The detail summary header is the display name as defined in the usage.
In the detail summary, dynamic records show two columns; the two fields of the record with the lowest display sequence. An edit icon is displayed, which provides access to a dialog that shows the full dynamic record(s). Dynamic fields are displayed in the much the same way. Rather than two, dynamic fields show a single column; the field value.
If URL dynamic logic was specified for a flex code field usage of a dynamic record, and that field is displayed in the summary, then that field will be displayed as a link. Clicking the link will open a new browser window with as URL the outcome of the dynamic logic function.
- Editing External Claims Data
-
Editing external claims data is done much in the same way as editing any claim header detail summary item.
Saving changes to external claims data works exactly like for other detail summaries: (1) Clicking 'Ok' in the external claims data dialog closes the dialog but does not commit the changes; (2) Changes are saved by clicking the save button on the claims page; (3) Clicking 'cancel' in the external claims data dialog closes the dialog and rolls back the changes made in that dialog. Changes made before the dialog was opened remain open.
Dynamic fields are edited in the much the same way. Note that the dialog only ever has a single column: the dynamic field value.
Access to external claims data (including the 'Exempt from Purging?' indicator) is governed by separate access restriction. This means that the function access restriction of the page that shows the external claims data does not apply its CRUD configuration on external claims data. To clarify, when a user has create rights on the enter claim page that shows the external claims data, but does not have create rights on the external claims data access restriction then that user cannot create external claims data.
If URL dynamic logic was specified for a flex code field usage of a dynamic record, then that field will have a link icon displayed next to its value. Clicking the link icon will open a new browser window with as URL the outcome of the dynamic logic function. Note that when the dynamic logic function uses the contents of the dynamic record to determine the URL, and the contents of the dynamic record are changed, the new URL will only be available after clicking OK in the dialog to process the changes.
- Displaying Dynamic Record Values
-
It is possible that the claim is extended with validated dynamic record values. These record values display in the same manner as external claims data dynamic record values, that is, as detail summary items that can be manipulated through a dialog.
Claim Line Section
This section displays the attributes of a claim line. The section holds the following fields in the table:
| Display Label | Entity Field |
|---|---|
Seq |
claimLine.sequence |
Start Date |
claimLine.startDate |
Qty |
claimLine.claimedNumberOfUnits |
(Procedure display name) |
claimLine.(procedure).code |
+ description |
claimLine.(procedure).description |
(Procedure 2 display name) |
claimLine.(procedure2).code |
+ description |
claimLine.(procedure2).description |
(Procedure 3 display name) |
claimLine.(procedure3).code |
+ description |
claimLine.(procedure3).description |
Modifiers |
claimLine.modifier.code |
Charged (Amount and Currency) |
claimLine.claimedAmount.amount and claimLine.claimedAmount.currency.displayCode |
Code |
claimLine.code |
The section holds the following fields in the inline overflow area:
| Field | Entity Field |
|---|---|
Line Ref |
claimLine.providerReference |
End Date |
claimLine.endDate |
Auth Exception |
claimLine.authorizationExceptionType |
Prio Auth No |
claimLine.authorizationCode |
Payer Paid (Amount and Currency) |
claimLine.precedingPayerPaidAmount.amount and claimLine.precedingPayerPaidAmount.currency.displayCode |
Entity Type |
|
Entity |
|
+ formatted name |
claimLine.servicedPerson.(formatted name) (Only for serviced entity type Person) |
+ description |
|
Entity Ref |
claimLine.providerEntityReference |
Servicing Provider |
claimLine.serviceProvider.code |
+ (formatted) name |
claimLine.serviceProvider.(formatted)name |
Service Specialty |
claimLine.serviceSpecialty.code |
+ description |
claimLine.serviceSpecialty.description |
Service Facility |
claimLine.locationProvider.code |
+ (formatted) name |
claimLine.locationProvider.(formatted)name |
Referring Provider |
claimLine.referralProvider.code |
+ (formatted) name |
claimLine.referralProvider.(formatted)name |
Pay To Provider[8] |
claimLine.paymentReceiverProvider.code |
+ (formatted) name |
claimLine.paymentReceiverProvider.(formatted)name |
Pay To Relation[8] |
claimLine.paymentReceiverRelation.code |
+ (formatted) name |
claimLine.paymentReceiverRelation.(formatted)name |
Location Type |
claimLine.locationType.code |
+ description |
claimLine.locationType.description |
The following claim line fields are mandatory:
-
claimLine.claimedNumberOfUnits (Qty)
-
claimLine.startDate (Start Date)
-
claimLine.sequence (Seq)
When entering a claim line the default value for the following check boxes is unchecked: Encounter?, Process as In?, Manual Pricing? and Manual Benefits?; these fields are not shown. The Emergency? indicator for each claim line is not shown and is set to the same value specified on the claim level whenever the Submit or Save button is clicked.
The status is set by Claims and can never be edited directly, this field is not shown.
The claim line sequence is re-sequenced each time a claim is saved or when it is submitted. re-sequencing is done prior to claim line code generation.
The claim lines codes can be entered manually or are issued by the system when saving or submitting a claim. Two approaches for code generation are possible:
-
If no dynamic logic of the signature 'Claim Line Code Generation' is defined, then claim lines codes are issued by the system with the format '1, 2, 3,…'. Except for the claim lines that already contain a manually entered claim line code: these codes are not updated.
-
If dynamic logic of the signature 'Claim Line Code Generation' is defined, then, claim lines codes are issued according to the logic specified in the signature. This updates any manually entered codes.
The claim line code is unique within a claim and is used for identification of the line. Claim line codes for claims that are not submitted can be edited in the Enter Claim page after which the same logic applies.
The claims form configuration defines:
-
The number of procedure columns shown (0, 1, 2 or 3)
-
The column header display names
-
The procedure code object field names
-
Against which flex code system the code is validated upon entry
Claim Line Detail Section
For each claim line detail, a 'display only' list of records is shown. These lists show a selection of key fields per detail records, for example, if a claim has ten diagnoses then all ten are shown with only priority, type and code.
The claim line detail section becomes scrollable when the accumulated height of all displayed records exceeds that of the claim line section.
All summaries display an edit icon. Clicking this icon will open a dialog that shows all information available for that claim line detail and allows the user to create line details for that claim line.
The subsections are listed in the same sequence as they appear (top to bottom) in the claim line detail section:
| Displayed Header | Remark |
|---|---|
Messages |
claimMessageList[].message.severity (only fatal claim messages are displayed) claimMessageList[].message.code (only fatal claim messages are displayed) claimLineMessageList[].message.severity claimLineMessageList[].message.code Edit/View icon |
Diagnoses |
claimLineDiagnosisList[].sequence claimLineDiagnosisList[].diagnosisType.description claimLineDiagnosisList[].diagnosis.code Edit/View icon |
Messages are sorted on code. Diagnoses are sorted on sequence.
Displaying Dynamic Record Values
It is possible that the line is extended with validated dynamic record values. These record values display in the same manner as external claims data dynamic record values on the claim header, that is, as detail summary items that can be manipulated through a dialog.
Messages
The user can attach a single message to multiple claim lines at once. First the user selects the claim lines to which the message needs to be attached - using the claim line selection check box - and clicks the 'Add Message' button. This opens the list of available messages. Messages that are Oracle Health Insurance-specific are not shown in the list. The user picks one of the messages from the list and clicks 'Ok'. The message is now attached to all selected lines.
The user can also delete one or more messages from multiple claim lines at once. First the user selects the claim lines from which the message is to be removed and clicks the 'Delete Message(s)' button. This opens the distinct list of messages that are currently attached to at least one of the selected lines. The user picks one of the messages from the list and clicks 'Ok'. The message is now removed from all of the selected lines to which it was attached.
It is also possible to attach and remove messages to and from lines through the claim line messages detail dialog. The user is free to add or remove any message.
Attributes on Multiple Levels
The following fields can be specified on either the claim or claim line and are visible on both levels:
-
serviced person or object
-
service provider
-
location
-
referral provider
-
diagnoses
-
service specialties
-
authorization code
-
payment receiver
-
location type
The following logic applies:
-
If the claim line field is unspecified, then it shows the value of its counterpart on the claim header level. If this field is also empty, no value is shown.
-
If the claim line field is specified, then that value is shown.
In context of these rules, the list of diagnosis codes is treated as a single field value. In other words, the user interface will not merge the set of diagnoses on the claim header with the diagnoses on the claim line; if the line specifies a list of diagnoses, those are the diagnoses shown for that line; if the line does not specify diagnoses, then the list on the claim header is shown for that line. Note that the display of the diagnoses values extends to the dynamic field values that may be specified on the intersection entities: claim diagnosis and claim line diagnoses.
Page Specific Rules
-
Only claims that have the status 'ENTRY' can be accessed through this page.
-
The following claim fields are updated accordingly, upon saving changes:
-
Total Claimed (Charged) Amount
-
This field is set to the sum of the claimLine.claimedAmounts (only non-replaced claim lines) as long as all the currencies of the claim line claimed amounts are equal; the currency for the total claimed amount is set as well
-
If the currencies are not equal the field is not set; if it was already set it is nullified (including the currency)
-
-
Start Date
-
End Date
-
-
The user is allowed to add informative and fatal messages with the exception of system specific messages. Added messages are attached as MANUAL messages.
-
The user is allowed to delete informative and fatal messages with the exception of messages that display only because they are actually attached to the claim header
-
When doing a cascade delete from a higher level (when deleting a claim line or claim), all claim line messages are deleted.
Header Buttons
The following buttons display on the top right of the page:
| Field | Remark |
|---|---|
Delete (icon) |
Deletes the claim. User is asked for confirmation with a dialog box. Confirmation will commit the delete. This is a cascade delete of all entities referring to this claim. |
Submit (button) |
Performs all steps of the save button. Sets the 'Pricing Done' indicator to 'No' (the indicator is not shown on the page) and saves the claim in the 'Initial' status, that is, the claim can no longer be altered and will be picked up for processing. It is checked whether the claim has at least one claim line; if not, then the claim status remains unchanged and the user is warned with a pop up message. The Enter Claim dynamic tab is cleared allowing entry of a new claim. |
Save (button) |
Saves the claim in the ENTRY status Set the 'Emergency?' indicator on all the claim lines. |
Cancel (button) |
Discards any unsaved changes and re queries the claim. |