Manual Benefits
See External Intervention for more information on manually applying benefits as part of the process flow.
This page describes altering the calculated benefit results through the Oracle Health Insurance Claims Adjudication and Pricing UI.
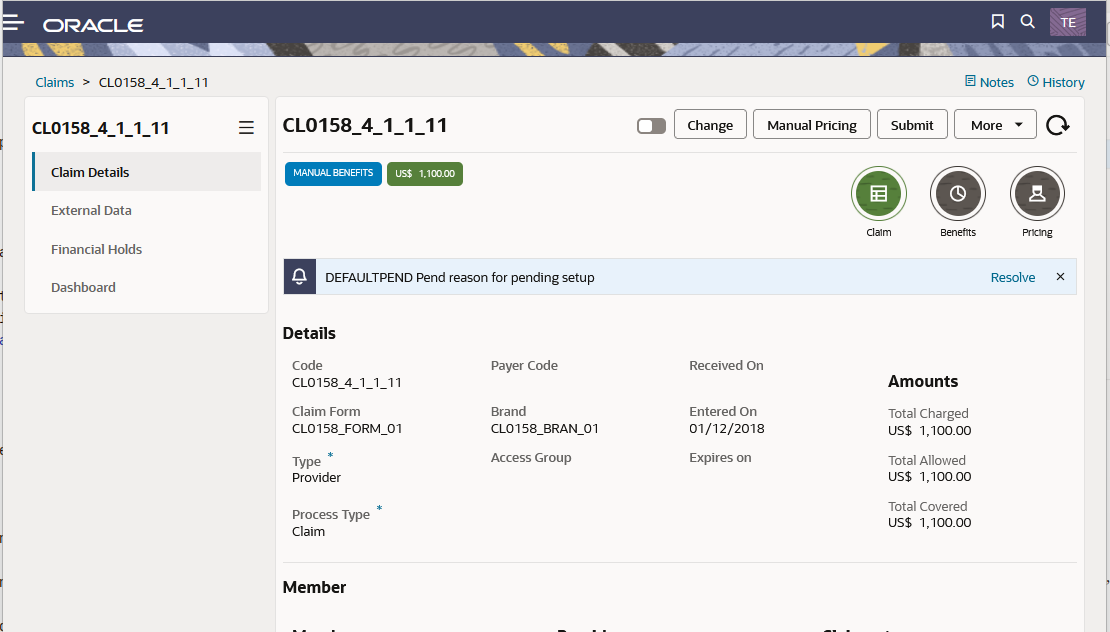
Oracle Health Insurance only allows manual adjudication of claims that have the status MANUAL BENEFITS [1].
Page Appearance
The page enables the user to add or remove external claims data and, on the claim lines:
Claim
The user can perform one of the following actions:
Change
The system reverts the claim to the CHANGE status. This makes it possible to change the claim, for example, changing the serviced person. [3]
This action uses the Back to Change http operation.
Manual Pricing
The system reverts the claim to the MANUAL PRICING status. This makes it possible to change the pricing results on the claim lines. [3]
This action uses the Back to Manual Pricing http operation.
Submit
The system saves the claim, sets the 'Pricing Done' indicator to 'No' and saves the claim in the 'Initial' status, that is, the claim can no longer be altered and will be picked up for processing.
The system checks whether the claim has at least one claim line; if not, then the claim status remains unchanged and the user is warned with a pop-up message.
After submitting the claim, the page re-opens in View mode with the claim in context.
This action uses the Submit Operation http operation.
Claim Details
The claim’s details are divided over the sections Claim, Benefits and Pricing. If the claim has unfinalize reasons they display in a separate section.
The top of the claim section displays pend reasons, messages and errors attached to this version of the claim.
For more information on these claim details see Claim details.
Claim Line
The user can perform one of the following actions on one or more claim lines.
Resolve Pend Reason
The system prompts the user to select a pend reason[4] and resolves the selected pend reason on all the claim lines where that pend reason exists. The system re-processes the claim.
This action uses the Resolve Pend Reasons http operation.
More
The More button enables the user to add a message, remove a message or add a pend reason to the selected claim lines.
The system prompts the user to select a message[5] or a pend reason.
After selecting the message or pend reason the system responds with an overview of the additions or removals it will do, and prompts the user to confirm (Submit).
Submitting the changes triggers a recalculation of the claim and refreshes the content of th page..
… Open
The Open option opens the claim line in a separate claim line window. This window shows the details of the claim line and supports a Manual Benefits button.
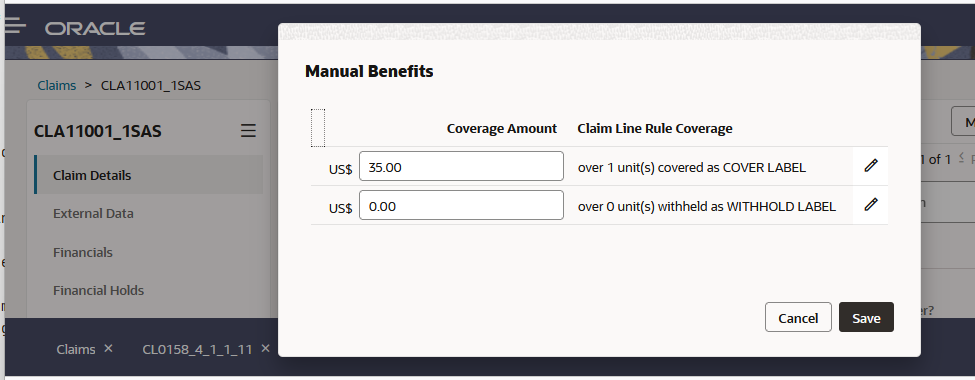
Selecting the Manual Benefits button opens up a window where the coverage amounts of this claim line can be updated. It is not possible to create or remove new coverages. It is not possible to change the currency of the coverage.
The system raises a fatal message if the user attempts to update the claim line coverages in such way that the sum of the coverages does not match the benefits input amount of that claim line.
Edits to the amount field may affect limit consumption.
| Code | Sev | Text |
|---|---|---|
GEN-UINT-025 |
Fatal |
The manual changes made to the claim line rule coverage can not be reconciled with the benefits input amount |
…Manual Benefits
The Manual Benefits option enables the user to change the coverage amounts of the claim line. See the …Open section above for more details.