Adjudication
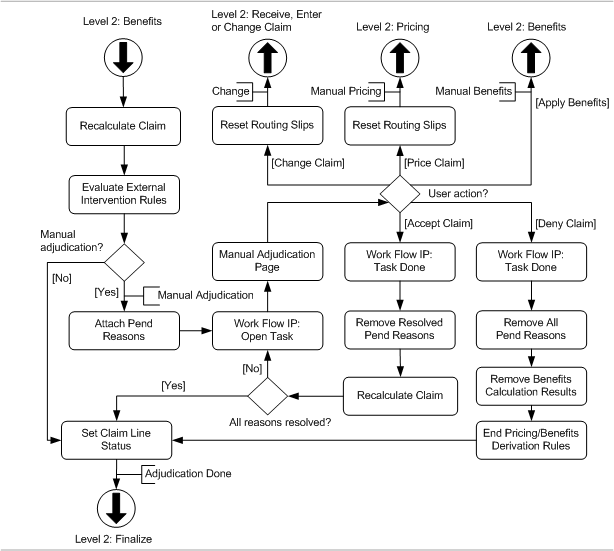
In this step the external intervention criteria for 'Manual Adjudication' are evaluated. At the end of the flow, the status of the Claim Lines is set. The adjudication flow is schematically depicted by the following figure:
Recalculate Claim
Claims that are both internally priced and adjudicated for benefits can sometimes trigger a recalculation. This happens if at least one claim line was successfully priced (no fatal messages attached during the pricing step) based on a provider limit (consumption with unchecked Ignored indicator is taken on a provider limit), but was denied after pricing (in the Set Claim Line Status step it is described when a claim line is denied). Because the line is denied, the consumption that it took during the pricing step is returned to the limit so that other lines - within the same claim - are repriced with that consumption available.
For these lines the Ignored indicator on the preliminary provider limit consumptions is checked and all results are kept. All other non-replaced and non-locked claim lines are recalculated based on their indicators:
| KP* | KB* | Action |
|---|---|---|
N |
N |
|
Y |
N |
|
Y/N |
Y |
Retain all results |
~KP: Keep Pricing Indicator, KB: Keep Benefits Indicator~
After the recalculation, the end-pricing (only if the claim was internally priced) and end-benefits derivation rules* are reevaluated and the total allowed amount and the total covered amount are updated accordingly if they had a value (not null):
-
total allowed amount is set to the sum of the claimLine.allowedAmounts of non-replaced claim lines
-
total covered amount is set to the sum of the claimLine.coveredAmounts of non-replaced claim lines
* Note that the claim line level rules are not evaluated for locked claim lines and replaced claim lines
Evaluate External Intervention Rules
First, the application checks if there are any existing pend reasons on the claim, bill and/or claim line level (there can be unresolved 'adjudication only' pend reasons); if this is the case the claim will be pended. After the 'existing pend reasons' check all external intervention rules of the sub type MANUAL ADJUDICATION are evaluated, regardless of already existing unresolved 'adjudication only' pend reasons. If a claim, claim line or bill successfully meets all of the criteria set by the rule, then the rule is 'triggered'.
For each triggered external intervention rule, the specified pend reason is checked: if the reattach indicator is unchecked and the pend reason history indicates that the same pend reason has been previously attached on the same level (claim, bill or line), then the pend reason is not attached and the claim will not pend because of this external intervention rule. Otherwise, the specified pend reason is attached to the claim, claim line or bill, and added to the claim pend reason history.
If no pend reasons are attached as a result of the external intervention rule evaluation, then the claim skips ahead to the "Set Claim Line Status" step. Otherwise, the claim status is set to MANUAL ADJUDICATION. See the implementation guide on claims flow configuration for more details on how to configure external intervention rules.
Manual Adjudication
If the claim is pended by a claim level external intervention rule with a checked Lock Claim Lines indicator, then all non-replaced claim lines of that claim are locked for any changes. If a specific claim line is pended by a claim line level external intervention rule with a checked Lock Claim Lines indicator, then that specific claim line is locked for any changes.
If the claim, claim line or bill has at least one pend reason with a checked 'publish message indicator', then the workflow integration point sends out a <task> event to notify a workflow management system that a new task is ready. The event contains all pend reasons that are configured to be published. For more detail, see the chapter on the workflow integration point in the implementation guide on claims flow configuration.
The assumption is that the external workflow management system assigns a manual adjudication task to a user. The user opens the UI page for manual adjudication and can choose to perform one of the following actions:
-
Accept the claim as processed by OHI Claims.
-
Deny a single line on the claim.
-
Deny the entire claim.
-
Revert to a status that makes it possible to change the claim, e.g., changing the serviced person.
-
Revert to a status that makes it possible to change the pricing results on the claim lines.
-
Revert to a status that makes it possible to change the benefits results on the claim lines.
Replaced claim lines and locked claim lines are ignored during this step, i.e., these lines will not trigger an external intervention rule for manual adjudication. It is still possible that the claim pends for manual adjudication triggered by other lines, the bill or the claim header. It is also possible that a locked claim line pends by an existing unresolved 'adjudication only' pend reason on the claim line.
Saving the claim
The manual adjudication page allows the user to change external claims data, add new claim line messages and deny individual claim lines. Denying a single line may affect the adjudication of other approved lines in the same claim. In order to make those changes apparent before accepting the claim, the user has the option to force a recalculation by saving the claim (this is described in more detail in the Manual Adjudication page description).
Saving a claim before accepting, provides the user with an opportunity to validate the recalculated results before the claim is released. Note that the user also has the option to deny one or more lines without saving first, before choosing one of the other available actions. Accepting the claim first saves the claim and therefore triggers the same recalculation as described above.
Changing the claim
This option returns the claim to the start of the claims flow, so that the fields on the claim itself can be changed. The claim indicators "Preprocessing Done?" and "Pricing Done?" are unchecked.
The claim status is set to CHANGE and it re-enters the level 2: Receive, Enter and Change Claim flow. Note that the claim, bill and claim line pend reasons remain attached.
Changing pricing results
This option sets the claim back to an earlier status in the flow so that the pricing results can be changed. The claim indicator "Pricing Done?" is unchecked. The claim status is set to MANUAL PRICING and it re-enters the level 2: Pricing flow. Note that the claim, bill and claim line pend reasons remain attached.
The claim pricing results can be edited in the "Manual Pricing" page.
Changing benefits results
This option sets the claim back to an earlier status in the flow so that the claim line rule coverages can be changed. The claim status is set to MANUAL BENEFITS and it re-enters the level 2: Benefits flow. Note that the claim, bill and claim line pend reasons remain attached.
The claim benefits results can be edited in the "Manual Benefits" page.
Accept Claim
When a claim is accepted, it is checked whether there is an open workflow task for that claim. This is derived from a technical field on the claim. If so, the workflow integration point sends out a message to inform the workflow distribution system that the task can be closed.
Next, any resolved pend reasons are removed from the claim, bill and claim line and the claim is recalculated (this is described in more detail in the Manual Adjudication page description). Note that these pend reasons are retained in the pend reason history. It is possible that one or more unresolved pend reasons remain attached to the claim, bill or claim line. If any pend reasons remain, the claim’s status remains MANUAL ADJUDICATION. If at least one of the remaining pend reasons has a checked publish message indicator, a new workflow integration point message is sent out. In effect, a claim will not be picked up by the process flow until all pend reasons have been resolved.
If no pend reasons remain, the claim continues on its way in the claims flow at the "Set Claim Line Status" step.
Deny Claim
When a claim is denied, it is checked whether there is an open workflow task for that claim. This is derived from a technical field on the claim. If so, the workflow integration point sends out a message to inform the workflow distribution system that the task can be closed. All pend reasons, both resolved and unresolved, are removed from the claim, bill(s) and claim line(s). The results of benefits are cleaned up (this is described in more detail in the Manual Adjudication page description).
After cleaning up the calculation results, the end-pricing (only if the claim was internally priced) and end-benefits derivation rules are executed a second time. The rationale is that those derivation rules are typically used to aggregate the results of the pricing/benefits calculation. Because the claim has been denied after the initial execution of the derivation rules, they have to be executed a second time. Both the end-pricing and end-benefit derivation rules are evaluated in the following order: claim line first, bill second, claim (header) last.
Set Claim and Claim Line Status
The status of a claim line is set to "DENIED" if one of following statements is true:
-
the claim line has no claim line coverages and has a product specific fatal message attached.
-
the claim line has a product independent fatal message attached.
-
the bill to which the claim line belongs has a fatal message attached.
-
the claim to which the claim line belongs has a fatal message attached.
Otherwise the claim line status is set to 'APPROVED'.
Note that the status of the claim line is not set if it is already set; locked claim lines can already have a status. If the status on locked claim lines is not already set, then it is set based only on the claim line messages; messages from higher levels are ignored.
The status of the claim is set to "ADJUDICATION DONE".