Manual Adjudication
This page allows a user to manually accept or deny a claim or claim lines. The page shows the same information as is visible in the View Claim page, with additional fields in the claim line section specifically for manual adjudication.
This page can be accessed through the Search Claim page by clicking on the claim code link on one of the search results or the "Adjudicate" button in the View Claim page. This will open an instance of this page in a dynamic tab for that particular claim. Alternatively, this page can be access directly by the URL provided in the work flow notification message.
Display and Specifics
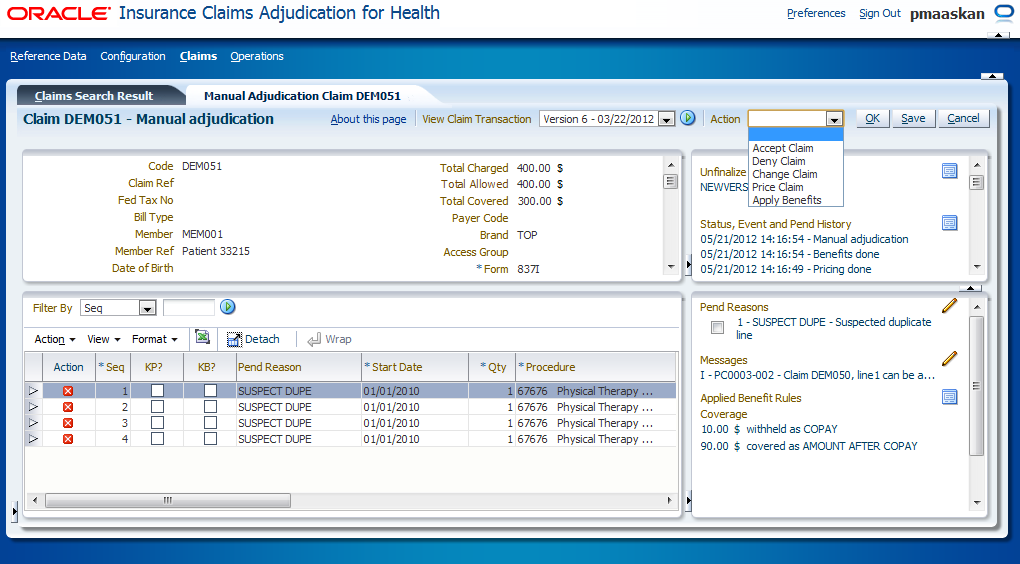
This page displays only claims with the status MANUAL ADJUDICATION. The page allows a user to deny an entire claim, or one or more individual lines.
Denying the claim
In order to deny the whole claim, the user clicks the "Deny" button. Then an LOV with messages appears. The LOV is filtered so that it only shows fatal messages that are not system specific. Once the user selects a message and hits the "OK" button in the LOV, the deny is committed and the selected fatal message is attached to the claim. The below specified actions are performed for all claim lines of the claim (except for locked claim lines and replaced claim lines).
The Keep Benefits and Manual Benefits indicators on the claim lines are unchecked, and the following calculated benefits results are discarded or set to zero:
-
Claim line covered amount (and thus the claim total covered amount)
-
The claim total covered amount is only set to 0 if it had a value (not null)
-
-
Claim line covered number of units
-
Claim line rule coverages
-
Claim line coverages
-
Claim line benefit specifications
-
Claim line messages with origin BENEFITS or COVERAGE
-
Preliminary authorization consumptions
-
The related authorization counter periods are also removed if no non-reversed consumptions remain under the periods (how consumptions count towards counter periods is described in the Authorizations implementation guide); the related authorization counters are also removed if no consumptions remain at all under those counters
-
-
Preliminary regime consumptions
-
The related regime counters are also removed if no consumptions exist any more under those counters
-
-
Preliminary limit consumptions
-
The related limit counter periods are also removed if no non-reversed consumptions remain under the periods (how consumptions count towards counter periods is described in the Adjudication Limits section of the Benefit Rules implementation guide); the related limit counters are also removed if no consumptions remain at all under those counters
-
-
Medical case details
-
The medical case details are removed because the claim is denied as a whole, implying that there is something wrong with the claim as a whole. The likely scenario is that the provider will send in a new, adjusted claim. To prevent the conflict of identical overlapping medical cases, the medical case has to be removed.
-
The values of the Keep Pricing and Manual Pricing indicators on the claim lines are kept, the Ignored indicator on the preliminary provider limit consumptions of the claim lines is checked and the calculated pricing results are kept:
-
Claim line allowed amount (and thus the claim total allowed amount)
-
Claim line allowed number of units
-
Claim line provider pricing clauses
-
Claim line messages with origin PRICING, PRICING LIMIT or PRICING NO RECALCULATION
-
Preliminary provider limit consumptions (the Ignored indicator on the consumptions is checked)
The end-pricing (only if the claim was internally priced) and end-benefits derivation rules* are reevaluated.
* Note that the claim line level rules are not evaluated for locked claim lines and replaced claim lines
Denying a claim line
In the claim line section (3), the action column shows a deny icon. This icon appears unless the line* either:
-
already has a fatal product-independant message attached
-
already has a fatal product-dependant message attached, but one or more claim line rule coverages exist
* The icon does not appear on locked claim lines and replaced claim lines
Clicking this icon opens up a LOV with messages. The LOV is filtered to show fatal messages that are not system specific. Once the user has selected a message and has closed the LOV dialog, the deny icon disappears for that line. Denying a single line may affect the adjudication of other approved lines in the same claim. In order to make those changes apparent before accepting the claim, the user has the option to force a recalculation by saving the claim. Saving the claim causes a recalculation of the entire claim (except for locked claim lines and replaced claim lines):
-
For lines that have been manually denied:
-
The Keep Benefits and Manual Benefits indicators are unchecked
-
The values of the Keep Pricing and Manual Pricing indicators are kept
-
The Ignored indicator on the preliminary provider limit consumptions is checked (this will ensure that these consumptions are ignored by other claim lines)
-
The following calculated benefits results are discarded or set to zero (note that medical case details are not removed):
-
Claim line covered amount
-
Claim line covered number of units
-
Claim line rule coverages
-
Claim line coverages
-
Claim line benefit specifications
-
Claim line messages with origin BENEFITS or COVERAGE
-
Preliminary authorization consumptions
-
The related authorization counter periods are also removed if no non-reversed consumption remains under the periods; the related authorization counters are also removed if no consumptions remain at all under those counters
-
-
Preliminary regime consumptions
-
The related regime counters are also removed if no consumptions exist any more under those counters
-
-
Preliminary limit consumptions
-
-
The calculated pricing results are kept:
-
Claim line allowed amount
-
Claim line allowed number of units
-
Claim line provider pricing clauses
-
Claim line messages with origin PRICING, PRICING LIMIT or PRICING NO RECALCULATION
-
Preliminary provider limit consumptions (the Ignored indicator on the consumptions is checked)
-
-
-
For lines that have not been manually denied:
-
For lines that have provider limit consumptions with a checked Ignored indicator: retain all results
-
For all other lines:
-
| EP* | KP* | KB* | Action |
|---|---|---|---|
Y |
Y/N |
N |
|
N |
N |
N |
|
N |
Y |
N |
|
Y/N |
Y/N |
Y |
Retain all results |
* EP: External Pricing Indicator, KP: Keep Pricing Indicator, KB: Keep Benefits Indicator
After the recalculation, the end-pricing (only if the claim was internally priced) and end-benefits derivation rules* are reevaluated and the total allowed amount and the total covered amount are updated accordingly if they had a value (not null):
-
total allowed amount is set to the sum of the claimLine.allowedAmounts of non-replaced claim lines
-
total covered amount is set to the sum of the claimLine.coveredAmounts of non-replaced claim lines
* Note that the claim line level rules are not evaluated for locked claim lines and replaced claim lines
Saving a claim before accepting, provides the user with an opportunity to validate the recalculated results before the claim is released. Note that the user also has the option to deny a line without saving first before choosing one of the other available actions. Accepting the claim first saves the claim and therefore triggers the same recalculation steps as described above.
Page appearance
All dialog boxes are display only, except for the claim and claim line pend reasons; new pend reasons can be added and the resolved indicator remains editable (only for non-replaced claim lines).
The claim line messages are editable as well (only for non-replaced claim lines); a user is allowed to:
-
add informative and fatal non-system specific messages (they will get the origin MANUAL)
-
on locked claim lines only informative messages can be added
-
-
remove informative and fatal messages with the origin MANUAL or EXTERNAL (except the messages copied from claim level)
-
on locked claim lines only informative messages can be removed Section 3 has the following additional columns:
-
| Display label | Entity, field |
|---|---|
Action |
Deny icon. Clicking opens an LOV with fatal non-system specific messages. |
Pend Reason |
Displays the claimLine.claimLinePendReason.code with the lowest value for claimLinePendReason.priority If the lowest priority value is shared by more than one claimLinePendReason, show the claimLinePendReason that comes first based on alphabetical sort on the pend reason code. |
To be |
Derived field* |
MP |
claimLine.indManualPricing |
MB |
claimLine.indManualBenefits |
*This fields gives a forecast of the claim line status for non-replaced claim lines and non-locked claim lines in the event that the claim is accepted. Since the claim line status is not set for claims in the status MANUAL ADJUDICATION, the value of this field is derived. If at least one of the following conditions is met:
-
the claim to which the claim line belongs has a fatal message attached;
-
the claim line itself has a non-product-specific fatal message attached;
then the value of the claim line "To be" field is set to "Denied" which means that the claim line is to be denied once the claim is accepted. Otherwise it is set to "Approved" which means that the claim line is to be approved once the claim is submitted.
Header Buttons
The following buttons are displayed on the top right of the local area:
| Field | Remark |
|---|---|
View Claim Transaction (drop menu) |
Provides access to claim transactions of the current claim. The drop menu contains one line for each claim transaction in the claims transaction repository that originated from this claim. Each entry shows the version number and transaction date. The most recent version is the default value. Versions are ordered by version number, most recent at the first entry. |
Go (Icon) |
Opens the View Claim Transaction page for the selected Claim Transaction. |
Change (button) |
Closes this page and opens (in the same tab) the Enter Change Claim page. |
Deny (button) |
Opens an LOV on messages. The user is required to select a fatal message that is to be attached to the claim. Committing the selected fatal message closes this page and opens (in the same tab) the View Claim page. The claim continues processing. |
Accept (button) |
The claim continues processing. If all pend reasons are resolved, this page closes and the View Claim page opens (in the same tab). A claim may only be accepted, when at least one change is made or when at least one outstanding pend reason is resolved. Also triggers the recalculation of the claim as described above. |
Manual Pricing (button) |
Closes this page and opens (in the same tab) the Manual Pricing and Benefits page. |
Manual Benefits (button) |
Closes this page and opens (in the same tab) the Manual Pricing and Benefits page. |
Refresh (button) |
Button that forces a re-query of the displayed claim. Used to track a claims status progress real time. |
Save (button) |
Saves any changes made to the claim (user is able to edit external claims data in this page). Also triggers the recalculation of the claim as described above. |
Cancel (button) |
Cancels any outstanding changes. |
The buttons 'Change', 'Manual Pricing' and 'Manual Benefits' set the claim back to an earlier part of the claims flow. The pend reasons on the claim and claim lines will remain attached; the application still considers the claim to be in a pended state. Resolved pend reasons are removed as soon as the claim is resubmitted for processing.