Reprocess Claims
The claim reprocessing page allows the user to reprocess claims based on a fixed set of criteria. Before submitting the request the user can determine the impact of the request which returns the number of claims, the total allowed and covered amount that would result from the provided criteria. When reprocessing a claim messages can be attached to the claim.
The Reprocess Claims page is accessible via operations menu. The page has three steps to submit the request:
-
Selection criteria
-
Reprocessing options
-
Review and submit
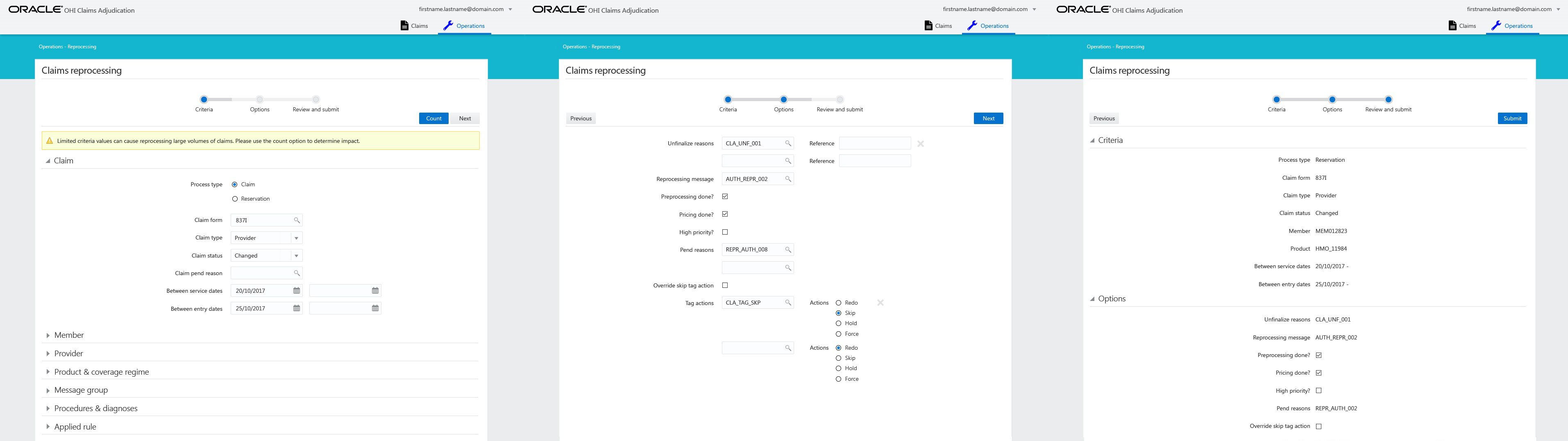
Selection Criteria
The following criteria are available for selecting claims. Only field process is mandatory:
Claim
-
Process type (mandatory)
The process type of the claim; claim, reservation or quote
-
Claim form, type & status
The claim line must belong to a claim of the specified claim form and claim type. The claim to which the claim line belongs must be in the specified status. Note that the possible status are confined to: CHANGE, MANUAL PRICING, MANUAL PRICING ADJUDICATION, MANUAL BENEFITS, MANUAL ADJUDICATION, PRICING FINALIZED and FINALIZED.
-
Pend reason
The claim and/or claim line must have a pend reason with the specified code.
-
Between service dates
The claim line start date must be between (inclusive) the specified start and end date.
-
Between entry dates
The claim entry date must be between (inclusive) the specified start and end date.
Provider
-
Benefits provider group
The claim line benefits provider must belong to the provider group on the service start date of the claim line. "Belong to" implies the same functionality that is used to determine whether a provider is in the scope of a certain provider group (an extensive description including examples, is given in the Benefits part of the claims flow).
-
Price provider group
The claim line price individual provider or the price organization provider must belong to the provider group on the service start date of the claim line.
-
Service provider group
The claim line service provider must belong to the provider group on the service start date of the claim line.
-
Location provider group
The claim line location provider must belong to the provider group on the service start date of the claim line.
-
Claimant provider group
The claim claimant provider must belong to the provider group on the service start date of the claim line.
Serviced Entity
-
Serviced entity type and code
The claim line serviced entity must have an insurable entity code and type code identical to the specified code and type. If there is only one insurable entity type configured, this type is used by default. In that case the type is not displayed in the UI. When entering only a type without an entity code it will be ignored when submitting the request.
Product & coverage regime
-
Product
The claim line has benefits applied from this product. Note that specifying a product in the request message implies that only those claims for which the benefits are actually applied are considered for reprocessing.
-
Coverage regime
The claim line has benefits applied from this coverage regime. Note that specifying a regime in the request message implies that only those claims for which the benefits are actually applied are considered for reprocessing.
Message group
-
Message group
The claim line must have a message attached that is in the specified message group.
Procedures & diagnoses
-
Procedure group
One or more of the claim line procedures must belong to the procedure group on the service start date
-
Diagnosis group
The primary claim line diagnosis must belong to the diagnosis group on the service start date. The primary claim line diagnosis is the diagnosis with the lowest sequence value.
Applied rule
-
Fee Schedule
The claim line is priced using a fee schedule line that belongs to this fee schedule.
Count
OHI can report back on the number of claims impacted from the selection criteria before submitting the actual request. A count button is present on the page. When clicked a count of the claims is returned as well as the total allowed amount and the total covered amount. This count is for informative purposes only; the count action will not reprocess any claims. OHI returns the count result in a UI information message. For example:
" These criteria will select 121 claims with a total allowed amount of $877.69 and a total covered amount of $632.12"
If either no total allowed amount or total covered amount is present the message is changed accordingly:
" These criteria will select 121 claims with a total allowed amount of $877.69"
or
" These criteria will select 121 claims with a total covered amount of $632.12"
When various claims have different currencies, only the count of the claims is displayed:
" These criteria will select 121 claims"
If the selection criteria is changed and the count button is pressed again, the previous count result is cleared and replaced by a new result.
Reprocessing options
In the second step the following reprocessing options are available:
-
Reprocessing message
This message code is attached to those claims that are reprocessed. Free text field. Optional, Default empty
-
Set to high priority?
Setting this attribute to the value Y(es) means that all reprocessed claims are marked as high priority claims. Checkbox. Default unchecked.
-
Set preprocessing done?
Setting this attribute to the value Y(es) means that the claim is not sent out for preprocessing. Checkbox. Default unchecked.
-
Set pricing done?
Setting this attribute to the value Y(es) means that the claim is not sent out for pricing. Checkbox. Default unchecked.
-
Override skip tag action?
Setting this attribute to the value Y(es) means that an existing tag action of Skip should be overruled. Checkbox. Default unchecked.
-
Claim unfinalize reasons
List of unfinalize reason codes
-
Claim pend reasons
List of pend reason codes
-
Claim tag actions
A list of tag/action combinations. The allowable values for the action are R (Redo), S (Skip), H (Hold) , F (Force) and U (Undo)
Review and Submit
The final third step displays the provided selection and reprocessing options . The request can be submitted from here. Only criteria and reprocessing options are displayed that have a value. This also includes all indicators.
Submit
Clicking the submit button will submit the criteria to the system for reprocessing.
If any errors would occur they are displayed in the UI. This means no claims will be reprocessed. The user will have to modify the request in order to submit again. If no errors are returned the the claims are queued for reprocessing. The results of the reprocessing process are not presented in the UI. Results are written to a data-file that can be downloaded by using the data file set integration point.