Pricing Overview
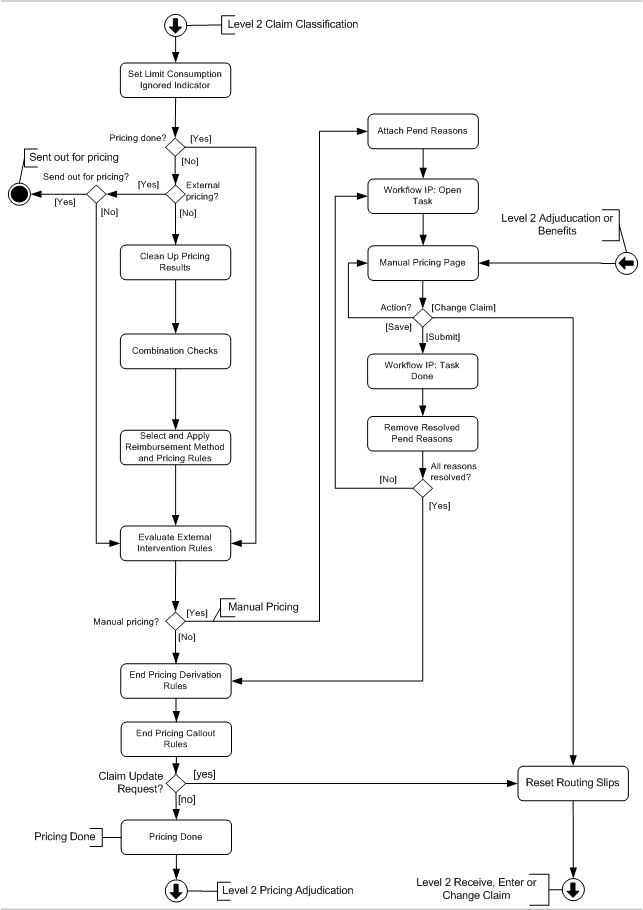
In this step it is evaluated whether a claim is already priced, whether it should be priced internally or if it should be sent out for repricing. After that, the external intervention criteria for 'Manual Pricing' are evaluated.The pricing flow is schematically depicted by the figure below.Note that the pend reasons that are specified in decision point 'All reasons resolved?' are pend reasons with indicator 'Adjudication Only' set to false.
Limit Consumption Ignored Indicator
The initial step of pricing is to set the Ignored indicator on the preliminary provider limit consumptions of all non-locked claim lines of the claim:
-
The Ignored indicator is checked for claim lines with a product independent fatal message of origin MANUAL, EXTERNAL, SANITY CHECKS, PRE PRICING, ENROLLMENT or RESERVATION (attached to the line itself, the bill or claim to which the line belongs).This will ensure that the consumptions are ignored by other claim lines (for example when a claim line that has provider limit consumptions is denied by a callout and is reprocessed).
-
The Ignored indicator is unchecked for all other claim lines.This will ensure that the consumptions are no longer ignored by other claim lines (for example when a claim line that has provider limit consumptions is denied in benefits and is reprocessed with a checked Keep Pricing indicator).
Pricing, where and when?
The purpose of this check is to filter any claims that have to be priced externally.This check is implemented by three consecutive evaluations:
-
Is this claim already priced?
-
Should this claim be internally priced?
-
Is the claim allowed to be sent out?
Pricing done?
There are two possible reasons why a claim does not have to be sent to a pricer module: either the claim has already been priced or the claim needs to be priced manually within OHI Claims.In both instances, the indicator pricing done of the claim should have been set to 'Yes'.
External pricing?
If the indicator external pricing of the claim has been set to 'Yes', the claim is meant to be sent to an external pricer.
Send out for Pricing?
If the claim field 'Ind Send Out For Pricing' is set to 'No', this prevents the claim from being sent out.This happens e.g. when externally priced claims should not be sent back for repricing.In effect, the combination of an indicator external pricing of 'Yes' and an indicator send out for pricing of 'No' leads to the same behaviour as pricing done set to 'Yes'.
When a claim is to be sent out for (re)pricing the following happens:
-
The claim gets the status SENT OUT FOR PRICING
-
The pre-finalized claim out integration point sends out a notification message that the claim is ready to be retrieved.
Once a claim gets the status SENT OUT FOR PRICING it will remain in that status until a new (priced) version of that claim enters OHI Claims through the claims in integration point.Send out for pricing is done irrespective of existing fatal messages
Keep pricing for claim line
If for a claim line the indicator Locked / Keep Pricing / Keep Benefits is equal to Yes then the claim line must not be (re)priced or evaluated for external intervention.This means that in that case the following steps are skipped:
-
Combination checks
-
Select and apply reimbursement method and pricing rules
-
Evaluate external intervention rules (for manual pricing)
If a claim line has a skip tag for allowed then the claim line must not be (re)priced.This means that in that case the following steps are skipped:
-
Combination checks
-
Select and apply reimbursement method and pricing rules
Clean Up Pricing Results
This step is described in Clean Up Pricing Results.
Combination Checks
Only combination checks with step 'Start Pricing' are evaluated here. These are combination rules that need to be evaluated before a reimbursement method or pricing rule can be applied, like checking whether a combination of claim line procedures is claimed that do not go together, e.g. both RENT and PURCHASE of a DME (Durable Medical Equipment).The messages attached by combination checks with step 'Start Pricing' have origin PRICING NO RECALCULATION.
Combination checks are not evaluated if a product independent fatal message (of origin SANITY CHECKS or ENROLLMENT) exists at the claim line, or at the claim or bill to which the line belongs.In addition, if the duplicate check attaches a fatal message to a claim line, then the evaluation of mandatory/exclusive checks of that line is skipped.
For further details, see the section on Combination Checks in the Pre Benefits Checks.
Select and Apply Reimbursement Method and Pricing Rules
This step is described in Select and Apply Reimbursement Method and Pricing Rules.
External intervention
All external intervention rules of the sub type MANUAL PRICING are evaluated. If a claim, claim line or bill successfully meets all of the criteria set by the rule, then the rule is 'triggered'.
For each triggered external intervention rule, the specified pend reason is checked: if the reattach indicator is unchecked and the pend reason history indicates that the same pend reason has been previously attached on the same level (claim, bill or line), then the pend reason is not attached and the claim will not pend because of this external intervention rule.Otherwise, the specified pend reason is attached to the claim, claim line or bill, and added to the claim pend reason history.
If no pend reasons are attached as a result of the external intervention rule evaluation, then the claim skips ahead to the "End Pricing Derivation Rules" step.Otherwise, the claim status is set to MANUAL PRICING. See the implementation guide on claims flow configuration for more details on how to configure external intervention rules.
Both replaced claim lines and lines with a checked "Locked", "Keep Pricing" and/or "Keep Benefits" indicator are ignored during this step, i.e., these lines will not trigger an external intervention rule for manual pricing.It is still possible that the claim pends for manual pricing triggered by other lines, the bill or the claim header.
Manually price a claim
If the claim, claim line or bill has at least one pend reason with a checked 'publish message indicator', then the work flow integration point sends out a <task> event to notify an external work flow management system that a new task is ready.The event contains all pend reasons that are configured to be published.For more detail, see the chapter on the work flow integration point in the implementation guide on claims flow configuration.
A work flow management system is responsible for assigning the manual pricing task to an operator.The operator uses page for manual pricing to work the claim.He or she can choose to perform one of the following actions:
-
Change the pricing results on the claim lines.
-
Change the claim itself, e.g., changing the serviced person.
-
Save any changes to the claim line allowed amount and/or allowed number of units (and recalculate the effect of the changes on provider limit consumptions and other claim lines) without resubmitting the claim for further processing.
-
Submit the claim for further processing.
Changing the claim
This option returns the claim to the start of the claims flow, so that the fields on the claim itself can be changed.The claim indicators "Preprocessing Done?" and "Pricing Done?" are unchecked.
The claim status is set to CHANGE and it re-enters the level 2: Receive, Enter and Change Claim flow.Note that the claim, bill and claim line pend reasons remain attached.
Saving the claim
Saving the claim will store the changes made to the allowed amount.The status of the claim remains MANUAL PRICING.
Submitting the claim
When a claim is submitted, changes are stored and it is checked whether there is an open work flow task for that claim.This is derived from a technical field on the claim.If so, the work flow integration point sends out a message to inform the work flow distribution system that the task can be closed.
Next, any resolved pend reasons are removed from the claim, bill and claim line.Note that these pend reasons are retained in the pend reason history.It is possible that one or more unresolved pend reasons remain attached to the claim, bill or claim line.If any pend reasons with indicator 'Adjudication Only' set to false remain, the claim’s status remains MANUAL PRICING. If at least one of the remaining pend reasons with indicator 'Adjudication Only' set to false has a checked publish message indicator, a new work flow integration point is message sent out.In effect, a claim will not be picked up by the process flow until all pend reasons with indicator 'Adjudication Only' set to false have been resolved.
If no pend reasons with indicator 'Adjudication Only' set to false (no pend reasons at all or only pend reasons with indicator 'Adjudication Only' set to true) remain, the claim continues on its way in the claims flow at the "Derivation Rules" step.
Derivation Rules
A derivation rule sets the value of certain fields on a claim, bill or claim line.At this point in the flow, only derivation rules are executed for which the "step" field has the value "end pricing".End pricing derivation rules are evaluated even if a fatal message is attached to the same (or higher) level as specified by the derivation rule.
The end pricing derivation rules are evaluated in the following order: claim line first, bill second, claim (header) last.The rationale behind this sequence is that end pricing derivation rules at the claim level thus can use results from end pricing derivation rules at the bill and claim line level.If multiple derivation rules exist for the same level, they are executed in order of the configured sequence (sequence null is evaluated last).
End Pricing Callout Rules
Callout rules may be executed in this step.The claim is sent back to status Change, if a callout rule is executed and the response to it contains a Claims Update request.Otherwise, the claim continues in the claims flow.
Callout rules are evaluated even if a fatal message is attached to (any level of) the claim.
Refer to the text on callout rules in the implementation guide on Process Rules.
Pricing Done
If during the pricing step a fatal message of origin PRICING, PRICING LIMIT or PRICING NO RECALCULATION is attached to the claim line (or inherited from higher levels):
-
The provider limit consumptions created during the evaluation of provider limit rules are removed (the created counters are removed if the removed consumptions were the only consumptions related to those counters).
-
If the origin of one or more of the attached fatal claim line message is PRICING or PRICING NO RECALCULATION, then all claim line messages that originated from provider limit rules evaluation (origin PRICING LIMIT) are removed.The reason is that these messages clarify calculation results that have been removed, and can therefore be removed themselves.
-
If the origin of all of the attached fatal claim line message is PRICING LIMIT, then only the informative claim line messages that originated from provider limit rules evaluation (origin PRICING LIMIT) are removed.
Note that the removal of consumptions and messages is not performed for locked claim lines.
The claim status is set to PRICING DONE. The "Pricing Done" indicator on the claim is checked.